

Discover more from HEALTH CARE un-covered
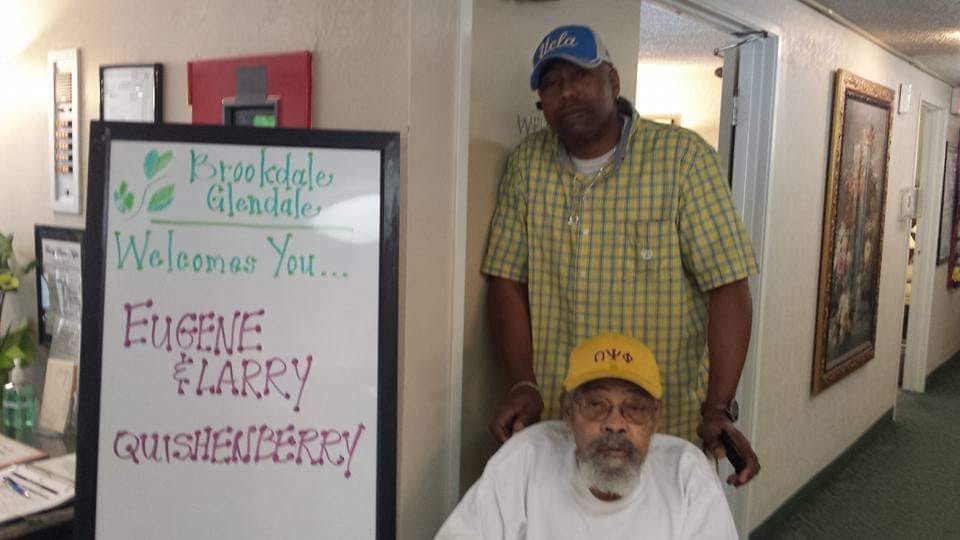
Eugene Quishenberry was 85 years old when his Medicare Advantage plan stopped covering his skilled nursing care. Less than a year later, in 2015, he died.
“It was weird. I came to visit him at the nursing home on Thanksgiving and they said, ‘Tomorrow we’re sending him home,’” his son, Larry Quishenberry, told HEALTH CARE un-covered.
“He hadn't been able to do rehab at all because he was laid up in bed with these pressure sores on his feet,” Quishenberry said. He was sent home even though he got the pressure sores while he was in the facility. “They never took care of the situation that was created in their place and sent him home anyway. He basically spent that last year in bed,” his son said.
Larry Quishenberry sued his father’s Medicare Advantage plan, asserting that he was improperly denied benefits that he was guaranteed under state law. The plan was run by UnitedHealthcare, which has 29% of the overall Medicare Advantage market. The case made it to the California Supreme Court, where it was dismissed: The justices held that the denial of care was not actionable under state law.
Eugene Quishenberry was African American. In the United States, one in four older Black and Latino adults report that they faced racial discrimination in health care, disparities that appear to be particularly acute in Medicare Advantage plans, which are approved by Medicare but operated by private insurance companies. As opposed to traditional Medicare, which works with almost all doctors and hospitals in the country and rarely requires pre-approval before medical services are provided, Medicare Advantage plans typically exclude many providers from their “networks” and often insist that doctors and hospitals get “authorization” in advance, resulting in widespread care denials.
A 2023 report conducted by RAND Health Care and funded by the Centers for Medicare and Medicaid Services found that “scores for Black Medicare Advantage enrollees were below the national average on 15 clinical care measures, similar to the national average on 19 measures, and above the national average on three measures,” with results even poorer for American Indian/Alaska Native populations.
Black and Latino seniors are more likely to be enrolled in a Medicare Advantage program than white seniors: 59% of Black seniors and 67% of Latino seniors are enrolled in Medicare Advantage plans, compared to 43% of white seniors.
A recent review of academic studies by KFF, a nonprofit health research organization, found that Black seniors in Medicare Advantage plans have been more exposed to preventable hospitalizations and readmissions, are not getting adequate access to mental health services, are less likely to see a specialist, and are more likely to be in a Medicare Advantage plan with lower star ratings.
A 2021 study by University of Pennsylvania and other researchers found that avoidable hospitalizations for Black seniors were more common in Medicare Advantage than in traditional Medicare, concluding: “Our findings provide evidence of racial disparities in access to high-quality primary care, especially in [Medicare Advantage].” The finding of avoidable hospitalizations buttressed a 2017 study finding that Black seniors in Medicare Advantage plans in New York state were twice as likely to be readmitted after major surgery as those in traditional Medicare.
Medicare Advantage plans have attracted scrutiny in recent months due to the reportedly frequent use of artificial intelligence to guide denials of care. Additionally, artificial intelligence in health care has been criticized for reinforcing racial disparities, with a 2019 study finding that an AI tool used by hospitals to predict care requirements understated the needs of Black patients. But as the KFF review notes, “Medicare Advantage insurers do not report data on prior authorization rates and denials by race or ethnicity, or the use of supplemental benefits for the overall Medicare Advantage population or by race or ethnicity.”
HEALTH CARE un-covered asked the Centers for Medicare and Medicaid Services (CMS) if they planned to begin collecting data that shows denial rates by race and ethnicity. CMS indicated that they currently have no plans to require the collection of this data.
Dr. Claudia Fegan works at the public Cook County Health System, where more than 80% of the patients are Black and Latino, and where, she says, Medicare Advantage plans have been wreaking havoc on her and her colleagues’ ability to provide the care patients need.
“I just got off of a utilization meeting, and the surgeons were complaining. So many patients are getting into Medicare Advantage. Then they need to have prior authorization. In Chicago, Humana only has one vascular surgeon in the entire Chicagoland area,” Fegan said.
“Humana will also not do provider agreements with the larger centers in Chicago. They may give you the facility but you can't use any of the providers in the network. The patients don't understand that they will have their care denied.”
Patients aren’t aware that their care will be compromised through Medicare Advantage, Fegan said.
“There’s a couple I've taken care of for 30 years. We went to the same high school. They signed up for a Medicare Advantage plan and they even pay for out-of-network benefits. They can be seen here at Cook County, but we can’t do anything with them,” Fegan said.
“The problem is that it’s too complicated a system for the average patient to navigate,” she said. “Patients with two college degrees can't navigate the system. Because poor people and people of color are the most vulnerable, they are the most susceptible to the problems inherent to Medicare Advantage’s rationing of care.”
Despite the problems that the expansion of Medicare Advantage has created for people of color, and Black seniors in particular, a selling point of the broader Medicare Advantage lobbying and marketing campaign is that it supposedly benefits Black seniors — with support even from some civil rights activists.
The head of the Wisconsin NAACP, Wendell Harris, endorsed the Medicare Advantage industry’s chorus against Biden administration proposals to limit Medicare Advantage spending in a March 2023 op-ed titled “Cutting Medicare Advantage Jeopardizes Vulnerable Wisconsinites.” Harris’ op-ed was trumpeted by the National Republican Senatorial Committee, which published a quick hit entitled “Wisconsin NAACP Slams Biden’s Medicare Cuts; Why Won’t Tammy Baldwin?” (Baldwin, a Wisconsin Democrat up for reelection in 2024, has criticized bad practices in Medicare Advantage.)
The Better Medicare Alliance, the main lobbying group for Medicare Advantage expansion, boasted that ”Medicare Advantage Is Closing the Health Disparities Gap for Seniors,” and argued that “minority seniors see benefit in Medicare Advantage for themselves.”
In a 2022 letter to CMS, a bipartisan group of members of Congress defended Medicare Advantage using the lens of racial equity, writing that “Racial and ethnic minorities eligible for Medicare also increasingly choose Medicare Advantage, with the greatest growth among Black and Hispanic enrollees.”
The National Caucus and Center on Black Aging, which includes William Clyburn, a relative of U.S. Rep. James Clyburn (D-S.C.), on its Board, announced at the beginning of 2023 in a report that “Medicare Advantage's supplemental benefits, better care coordination, and cost savings are particularly meaningful” for African-Americans.
Targeted Marketing
Medicare Advantage plans have aggressively targeted Black and Latino seniors through their marketing campaigns.
“Seniors are being bombarded by people they know from younger times — William Shatner, Tom Sellick, JJ Walker,” Fegan said. “They get people they're familiar with. They tell them these are great plans.

“They are being manipulated. They tell them you can get a broker. They don't tell them that the broker gets paid so much more to get you into Medicare Advantage than a Medigap plan. Then each year you renew they get a bonus. That’s deceptive advertising.”
She blamed the insurance industry’s lobbying group, America’s Health Insurance Plans (now known as AHIP), for the enthusiasm for Medicare Advantage in Washington. “Congress bought this hook, line and sinker without realizing they’ve been taken for a ride by AHIP.”
Subscribe to HEALTH CARE un-covered
Pulling back the curtains on how Big Health is hurting Americans and how we got to this point.

















A major issue here is that the cost of alternatives to MA for lower income seniors is usually unaffordable. When offered a choice between a so called $0/ mo premium and several hundred dollars/mo for a Medi-gap plan, why would an uneducated consumer of any race choose the latter ? And how could even an educated senior consumer afford it unless they had a pretty middle class life and income? MA ads need to come with a health warning like cigarette packs.
And now many retirees with health coverage are being forced into MA plans. Really bad.