

One of the worst moments for Logan Coulter this summer, at the rock-bottom low point of his 13-year-old daughter Gianna’s long-running health crisis, came when his two different worlds of agony collided with each other.
The Melba, Idaho, father of three was yet again bouncing from person to person on the phone with customer service representatives from Cigna, his health insurer – desperately trying to say the right words or find the right person who would finally understand the importance of approving coverage for a costly but proven-effective treatment for Gianna’s rare debilitating inflammatory brain disorder.
Meanwhile, Gianna was in the room next door – bedridden and sometimes writhing and shouting out in pain from the disorder known as PANS, or Pediatric Acute-onset Neuropsychiatric Syndrome.
Hours earlier, the deeply religious father and daughter had yet again said the rosary together, which often caused her symptoms to calm for a while. But now, as Coulter sat at his desk on hold with Cigna, pleading to speak with a decision-making doctor who might authorize infusion treatments for Gianna, the middle schooler was screaming out.
“‘Daddy, I don’t feel good’,” Coulter recalled, tearing slightly as he often does when he recounts his little girl’s ordeals. “‘Can I just go to heaven?’ She was just in agony, and I couldn’t even get a human on the phone.”
The Coulter family’s long-running battle to get Cigna – the nation’s 15th largest corporation – to cover what the leading medical authority on PANS had told them was the only drug with any hope to alleviate her suffering was an extreme example of a kind of trauma that millions of Americans face all too frequently.
A 2023 study by the health site KFF found that roughly six of ten Americans covered by health insurance nevertheless had trouble with a claim – most commonly because of the process known as prior authorization. That’s how companies like Cigna say they determine whether an expensive drug or procedure is truly necessary. Investigative reporters for sites like Pulitzer Prize-winning ProPublica have found that claims and preapproval requests – sometimes for life-altering treatments – are frequently rejected with little or no consideration, often by doctors with no expertise in the medical issue the patient is experiencing.
But Gianna’s story turned out differently for two reasons. One was the dogged persistence of her family who – unlike the vast majority of Americans turned down by Big Insurance, who do take “no” for an answer – kept calling Cigna and appealing through their specialist doctor more than 1,000 miles away in Indiana before eventually turning to contacts on social media in their desperation to find anyone who could help.
The other X factor was good luck. The initial plea from Logan Coulter – an executive with a real-estate title firm – to his mid-sized following on LinkedIn caught the attention of an executive working on solutions to the prior authorization crisis, who sent it to prominent people he knows, including the popular billionaire owner of the Dallas Mavericks, Mark Cuban. Soon, Cuban was retweeting at Cigna on Gianna’s behalf, and the now-viral social media campaign was also boosted by Hollywood actors Angie Harmon, Jeremy Renner and Harold Perrinau from TV’s Lost, who even texted Coulter to tell him that his own daughter had also struggled with PANS and understood the family’s ordeal.
The celebrity-backed campaign succeeded in ways the Coulters’ efforts – as an average American family – did not. Not long after Coulter’s second video about Gianna was posted, a woman from Cigna called to announce that she would be the girl’s case manager. Not long after that, the insurer said it was approving her treatments known as IVIG – for intravenous immunoglobulin, an infusion of antibodies – for three-month intervals going forward, and even would retroactively reimburse for a $15,000 first round that Coulter had paid from his own pocket.
We spoke with Coulter roughly 24 hours after the good news from Cigna, and he told us there’s a lesson for so many others who’ve been denied coverage for necessary treatments.” If you get denied, use that fight you have in yourself,” he said. “Don’t accept a denial…You will prevail if you use the love and passion that you have. Keep clawing and scraping.”
This one determined dad proved that can work, but the American health care system should never make it this hard in the first place.
The family’s ordeal began with a medical mystery. About two years ago, everyone in the Coulter household – including Gianna’s two brothers, Heston and Callum – began to suffer strange illnesses around the same time, Coulter’s wife would find herself shaking, while their 10-year-old Callum was experiencing nausea and dizziness in school.
No one seemed more ill than Gianna, a normally outgoing middle schooler with a great sense of humor and a love for sports – especially soccer, which she played on travel squads while dreaming someday of a pro career. But everything changed. Recalled her dad: “Gianna had it the worst – especially at night. She was in an altered state of mind – angry, crying, saying that [her] brain didn’t feel right.”

Finally, Callum’s pediatrician determined after some tests that toxic mold was the likely culprit, and the family learned that an attic at home was thoroughly contaminated. The Coulters moved, and the ailments were treated and cleared up – except for Gianna. Over the next year or so, the girl’s outbreaks grew longer in duration.Local doctors in Idaho were initially flummoxed until finally, one raised PANS as a possibility.
PANS is a rare disorder that occurs usually when some other trigger, like an infection, sparks the immune system. It often appears suddenly in young people, and it can bring a variety of symptoms including mental health problems – such as obsessive-compulsive or eating disorders for some – or issues like the extreme irritability, pain and speaking and writing problems that Gianna experienced.
The determined Coulters looked for the top national expert on PANS. When they learned he was two days away they got in their vehicle and drove to Carmel, Indiana, to meet Dr. Scott Antoine, who wrote the book on the syndrome – literally. Antoine’s battery of tests confirmed a PANS diagnosis. Afterr a series of more conventional therapies like antibiotics and steroids showed little improvement, Antoine said IVIG was probably her only hope for relief. The infusions are not cheap – about $15,000 for each monthly dose – and when the treatment plan was submitted to Cigna, it was initially denied as “experimental.”
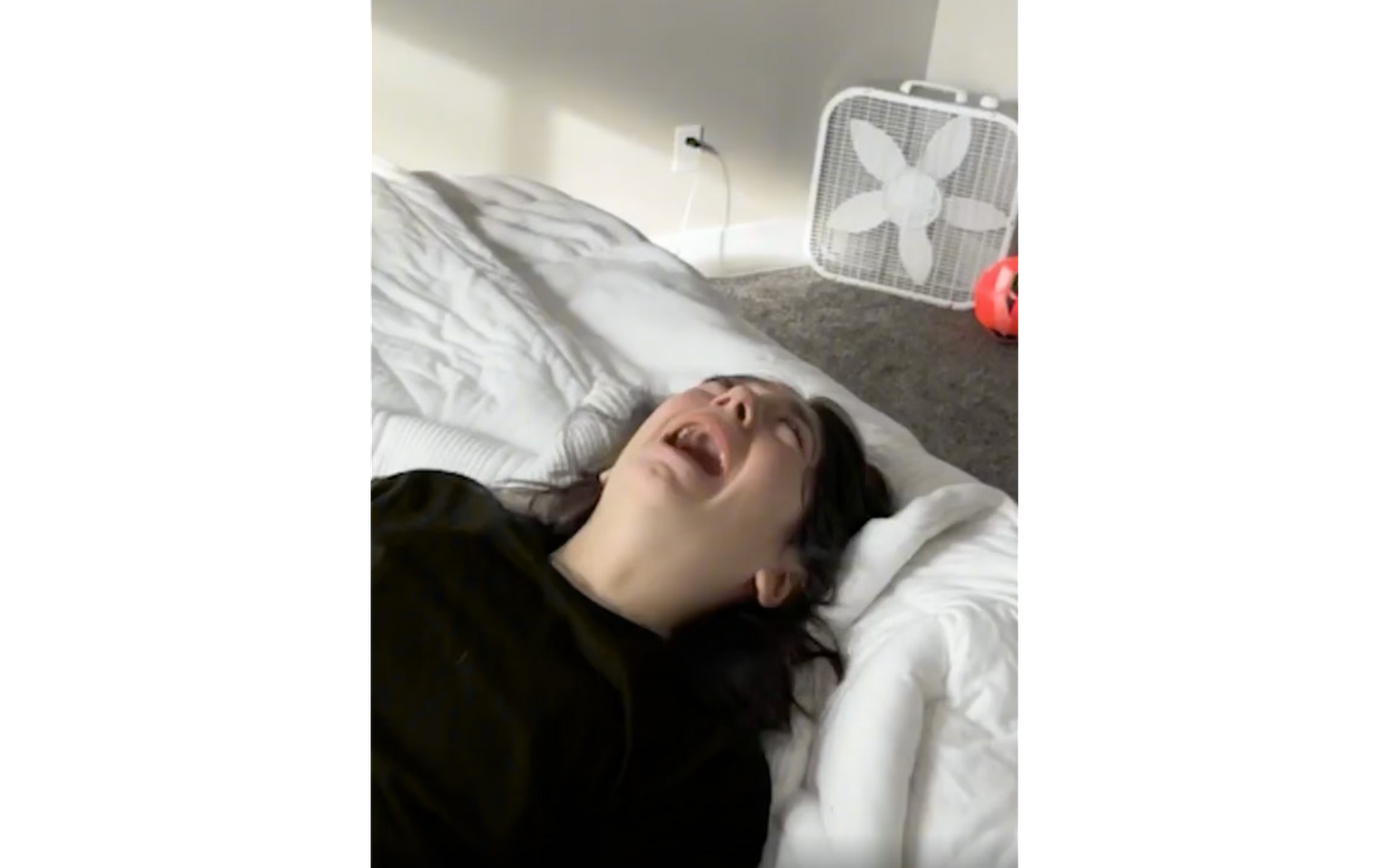
The next few months would be agonizing ones for the Coulters – especially with their awareness that medical relief for Gianna was a possibility. Instead, her condition worsened while the family and their physician labored to explain that the IVIG infusions – which had proven successful in other PANS patients – weren’t experimental but the only viable option. Gianna’s flares by then were lasting most of the day and keeping her awake at night, often leaving the once-star athlete unable to speak. In a gut-wrenching video, Coulter showed a scrap of paper where she tried to ask for “mac and cheese” but could only scrawl a couple of letters.
Meanwhile, Cigna denied an appeal that Coulter said was reviewed not by an expert on PANS but by an allergist. Antoine then sought and received a medical peer review which he thought would certainly change the insurer’s mind, yet it didn’t. Coulter said at this point he decided – belatedly, in his thinking – to start paying out-of-pocket for Gianni’s IVIG, even after calculating that $175,000 over two years would devastate any life savings. He said Gianna saw immediate progress after the initial treatment earlier this fall, with a couple of long periods of lucidity and shorter flares after that, giving the family hope.
But the Coulters never abandoned their other hope: Getting Cigna to cover the treatment. The reaction to Logan Coulter’s first LinkedIn video was more than he could have ever expected. One of those responding was Warris Bokhari, CEO of the startup company Claimable which is fine-tuning artificial intelligence to help patients and their doctors appeal prior authorization denials. Not only did he help Coulter draft a new appeal to Cigna, but it was Bokari who reached out to the popular Cuban, who has 8.9 million followers on the social media platform X.
On Nov. 10, Cuban retweeted Bokhari’s plea for Cigna to approve Gianna’s IVIG, which opened the floodgates not only for endorsements from other celebrities but also engaged the CEO of the national parent company of Coulter’s title-firm employer in the push. Cigna reached out to assure Coulter it would honor the three-day window on deciding their appeal, then approved the treatment, including the retroactive coverage of the first round that Coulter had sprung for.
Coulter didn’t have much time to bask in the victory. The family was packing for another long drive to Indiana to consult with Antoine, then back to Idaho for Gianna’s next infusion. Both the family and those who advocated for the 13-year-old know their saga is only a “feel good” story up to a point.
Most physicians and health care advocates believe the entire system of prior authorization needs a sweeping overhaul. The Biden administration enacted some significant reforms, but only for Medicare Advantage programs. Lawmakers on Capitol Hill and in several state legislatures continue to push for new measures to rein in the worst abuses by insurance companies.
After all, Mark Cuban can only tweet about so many cases. Even Gianna Coulter, a 13-year-old now seeking to put her personal ordeal in the rearview mirror, understands this. Her father said Gianna’s first reaction when she heard Cigna had authorized her care was to say: “Daddy, what about all the other kids?”
]]>
In 2018, Congress passed the VA MISSION Act, which was celebrated as a pathway to expanding veterans' access to health care, theoretically giving them a choice to see private providers when the VA couldn’t meet their needs. However, the reality of this privatization effort has been less about expanding choices and more about lining corporate pockets at the expense of veterans, their families, and American taxpayers. If you look closely, you’ll see how some of the very same companies behind the Medicare Advantage scheme — like Optum, a subsidiary of UnitedHealth Group — are cashing in on both fronts.
The MISSION Act opened the doors to the Veterans Community Care Program (VCCP), enabling veterans to receive care from private providers if they couldn't access VA services within certain time or distance constraints. In principle, this might sound like a good idea, but, in practice, the implementation has drained funds from VA facilities, creating a vicious cycle. The more funding diverted from the VA, the harder it is for veterans to get the care they need within the VA system. This drives even more veterans into private care, feeding the expansion of a system that has proven to be more costly, fragmented, and, as research now shows, riddled with fraud.
Consider the role of UnitedHealth Group’s Optum in this arrangement. Optum is one of the third-party administrators for the VCCP tasked with managing this vast network of private providers, a role that earns UnitedHealth billions of taxpayer dollars. Yet that’s not the only way this huge corporation profits from veterans' health care. For veterans enrolled in private Medicare Advantage (MA) plans run by UnitedHealth, Optum effectively double dips — collecting full payments from Medicare for the expected medical costs of that enrollee for the entire year while simultaneously charging the VA for coordinating private care for the same patient. According to a recent study from Harvard, as much as $1.3 billion in excess funding went to Medicare Advantage plans for veterans who, by and large, relied on VA care instead. Opening the door for Big Insurance to administer VA health coverage has created three interconnected issues:
It allows insurance companies to get payments from the government for care they exaggerated or did not provided
It allows insurers to use the same playbook they use in MA
It drains funding from the publicly administered VA health system
To understand why this matters, consider how Medicare Advantage has become a profit engine for private insurers, often without delivering adequate care to its members. These plans receive large per-patient payments from the government, intended to cover care for the year. However, the Harvard study found that nearly one in five veterans enrolled in Medicare Advantage plans received no Medicare-covered services despite these plans collecting full payments. When companies can make billions for services they aren’t providing, there’s little incentive to improve care. Big Insurance has caught on to this trend and has created plans that insurers specifically market to veterans to increase the number of veterans in their MA plans. Big Insurance perversely markets these plans as a benefit you can get because you served your country, but the plans are really just a way for insurers to make more money.
Optum’s role as a third-party administrator for the Veterans Community Care Program takes the same troubling trend in a new direction. Optum assembles and oversees private providers who often bill high rates for simple services or engage in“upcoding” to inflate charges. These are the same tactics we and others have been sounding the alarm about in Medicare Advantage for years.
In 2022, Suzanne Gordon, senior policy analyst at the Veterans Healthcare Policy Institute and co-author of ‘Our Veterans: Winners, Losers, Friends, and Enemies on the New Terrain of Veterans Affairs,’ wrote in The American Prospect that between 2017 and 2020, spending on non-VA evaluation and management services under the Veterans Community Care Program surged by 500%, with rampant upcoding uncovered by the VA’s Office of the Inspector General (OIG).
The problem with turning veterans’ health care into a corporate profit center is that private corporations, like UnitedHealth, are accountable first to their shareholders, not to the veterans they serve. Studies have shown that veterans enrolled in VA health care generally fare better in terms of outcomes and patient satisfaction than those seeking care in the private sector. Yet, by shifting more veterans into private care networks, we are reducing funding for the VA’s dedicated facilities and staff, eroding the very system that was built to serve veterans and leaving them vulnerable to profiteering by companies that view them as revenue sources.
Moreover, private providers working within the Veterans Community Care Program have few quality controls or accountability measures, as highlighted by the OIG. Many of these providers, shielded by a fragmented system, bill the VA without providing the expected standard of care, and no one is there to stop them. The OIG’s recommendation for more training in billing accuracy falls woefully short of addressing the systemic exploitation at play.
Privatization in veterans’ health care reflects a larger trend in the American health care system — one in which privatized entities reap maximum profits from government funds while taxpayers foot the bill and patients face gaps in care. It’s a phenomenon we see in Medicare Advantage, with private companies skimming billions by exploiting loopholes. We are now witnessing the same strategy in veterans’ health care.
Veterans deserve a health care system that is centered on them, not corporate profits. It’s time for Congress to take a hard look at the MISSION Act’s consequences, with an eye toward reining in abuses and restoring the VA’s core funding and capabilities. Veterans did not sign up to become another line item on UnitedHealth’s balance sheet. They deserve better than a system in which the government hands over billions without meaningful oversight or accountability.
As taxpayers and citizens, we must insist that our government protects veterans and honors their service by safeguarding the very system meant to care for them. Congress should take steps to stop these harms to the VA, starting with ensuring that Big Insurance companies do not receive full MA annual payments for their veteran enrollees who get their care at the VA. It’s time to end the privatization experiment in VA health care and return to the vision of a well-funded, publicly accountable system that values health over profits.
]]>
When I saw that CVS Health had replaced Karen Lynch with David Joyner as CEO and brought in Steve Nelson — a former UnitedHealthcare executive — to lead its Aetna subsidiary, I felt a mix of familiarity and concern. Karen and I go back to our days at Cigna, where both of us, along with people like David Cordani (now CEO of Cigna), climbed the corporate ladder. Back then, we shared a front-row seat to the early days of high-deductible “consumer-directed health plans” (CDHPs)—plans designed to shift more costs to patients while letting insurers pay out less in claims.
At Cigna, Karen, David, and I – along with several other corporate leaders – were tasked with pushing this concept, promoting the idea that patients would become “prudent health care consumers” if they had more “skin in the game.” The reality, however, was that these high-deductible plans meant many Americans, including our own employees, would end up skipping care, abandoning prescriptions, or even going into debt. But we had our marching orders, and corporate America had its agenda: reduce claim liabilities while selling “consumer empowerment” as the solution.
Now, CVS’s decision to bring in Nelson to lead Aetna – and promote Joyner to replace Karen as CEO – feels like a return to the same playbook. Nelson’s track record at UnitedHealth — a company that has vertically integrated into nearly every aspect of the health care landscape — suggests that CVS is hoping to expand its grasp on the marketplace. This move aligns with pressure from activist investors, like Glenview Capital Management, that have been calling for CVS to cut costs. Cutting costs can come in the form of paying fewer claims – and circumventing the medical loss ratio by “self-dealing” services to companies CVS owns.

Wall Street welcomed the change in leadership and strategic direction with a 13% jump in CVS shares, but we must ask—at what cost to patients? Aetna’s Medicare and Medicaid plans, which provide coverage to millions of people, are particularly at risk of being squeezed under this new leaders’ mandate to improve financial performance.
Take the third quarter financials. CVS reported a medical loss ratio of 95.2% — meaning that a higher than expected percentage of premiums had been used to pay claims, leaving less money to reward shareholders. The MLR was far higher than in previous quarters – and much higher than Wall Street had expected – and signaled that the company underestimated medical costs. That disclosure led to a massive selloff of the company’s shares. To get back into investors’ good graces, the company has embarked on an ambitious strategy to cut expenses. For those on Aetna’s Medicare Advantage plans, higher deductibles, more restrictive networks, and more aggressive use of prior authorization could be in their future, putting essential care further out of reach.
When Karen and I were helping to implement so-called “consumer-driven” plans, we knew what was at stake. These high-deductible plans made working Americans pay more upfront, while big insurers enjoyed record profits.
With CVS’s leadership team’s focus on “performance and value creation,” the company is signaling a renewed and absolute commitment to shareholders first, leaving patients to navigate the growing complexities – and costs – of their health care.
]]>
In the winter of 2011, I walked away from fifteen years of training in surgery and psychiatry, working in both rural and urban emergency rooms, and as a private practice psychiatrist, to manage research funding for the U.S. Army in regenerative medicine and hand and face transplants. I was exhausted and frustrated that, on too many days, no matter the delivery structure – academic, state-funded, or private practice – it was nearly impossible to get my patients the care they needed. I grieved for the only career I’d ever wanted and had worked so hard to achieve, but being complicit in a system that borrowed my credibility and exploited my patients’ vulnerability to serve its own purposes was nonnegotiable. I had to leave but one question lingered: Resourceful and resilient in every other area of my life, why couldn’t I make this doctoring thing work?
Four years later, I began exploring that question in earnest, after learning about a Midwest physician’s death by suicide. Physician colleagues across the country in various specialties and practice structures eagerly told me, informally and in confidence, about their work experience and their distress. Repeatedly, I heard the same refrain: “I signed up to work long hours and to see impossibly difficult things. What I didn’t expect was how hard it would be to get my patients the care they need.” These colleagues rejected burnout as an inaccurate description of their experience because the term implied individual susceptibility to the pressures of the job but said nothing about the endless, maddening challenges built into systems of care that made it hard to uphold their oaths. They needed different language, but what?
One steamy spring day about a year into this journey, I heard a research psychologist on NPR talking about his work with military veterans who suffered a different kind of invisible wound from post-traumatic stress. They had a compromised sense of their moral integrity, rather than their sense of physical safety. He called it, “moral injury.”
The term, first used with combat veterans, refers to the perception of betrayal by a legitimate authority in a high stakes situation that causes one to transgress deeply held moral beliefs.
The veterans with moral injury felt like they lost their moral compass. In health care, the deeply held beliefs referenced in the definition are the oaths we take to put patients first. The description of moral injury sounded like what I had heard from colleagues who described a conflict between carrying out their oath to heal and keeping their jobs in a profit-driven system. Caught between conflicting demands, these doctors, like soldiers, were questioning their moral core.
One of the first colleagues I ran this concept past was Simon Talbot, a reconstructive plastic surgeon who specializes in hand surgery. We met because of a shared interest in hand transplants, but our vantage points in medicine were very different. Simon was a surgeon, and I was a psychiatrist. He worked in academic medicine, and I walked away from a private practice. He left New Zealand after medical school, so he was steeped in publicly funded universal health care. And, whereas I come from a long line of salesmen and plumbers, medicine is in his blood — his great grandfather, grandfather, father, uncle, and twin sister were doctors; his mother and her mother were nurses. We talked between sessions at a transplant conference in 2016 about how medicine changed us. We soon concluded that, if our experiences were so similar, despite our many differences, then we probably were not the problem, the system was the culprit. Moral injury struck him, too, as an accurate descriptor of his experience.
Our conversations might have gone nowhere except that when I returned home, my physician husband’s stable congenital heart condition suddenly and rapidly deteriorated. The local physicians, who were also my husband’s colleagues, were inexplicably paralyzed. They dragged their feet about making plans to transfer him and I watched, helpless and imploring them to intervene, as a terrifying critical illness almost ended tragically. They finally sent him to a teaching hospital two hours away and he recovered fully, but I was deeply puzzled and vowed to understand why those local physicians, who I knew were good people, took so long to act in their patient’s best interest. It turned out that a new corporatized mindset was behind their delays, keeping every justifiable dollar from leaking out of the health system. Those physicians had to play brinksmanship with my husband’s life or risk their jobs.
A few months later, armed with firsthand experience of the impact on patients, Simon and I laid out our concept of moral injury to a group of academic surgeons. We proposed that the demand-resource mismatches of burnout contributed to clinician distress, but the policies and management practices running counter to our oaths, and heedless of patient best interests, was most of the problem. Physicians are skeptical scientists, to the core. We expected they would approach this new idea with reservations and poke holes in the concept. If they did, it would only make our planned paper stronger. Instead, almost in unison they paused, raised their eyebrows, and then rattled off story after story of how moral injury fit their experience. They unanimously urged us to publish it.
Many months and many rejections later, STAT News published our paper. Immediately, emails, direct messages, and calls flooded in. Most were some version of, “This is the language I’ve needed for years.” We waited for interest to die down, but instead, it grew and spread beyond health care, to social workers, veterinarians, teachers, public defenders, and others who felt the language also applied to them. So, in the fall of 2018, we established a nonprofit organization, Moral Injury of Healthcare, to change the narrative of occupational distress. Dozens more articles, research papers, a book (If I Betray These Words), and two podcasts have followed, and “moral injury” is now a widely used descriptor of occupational distress. But the systemic and cultural changes that form the core of solutions are meeting resistance at many levels of leadership.
Clinicians commit years to learning their professions, during which it is ingrained that patient needs always take priority. In exchange for their courage and persistence, they want the autonomy and latitude to provide excellent care and comfort, in accordance with their training. Moral Injury of Healthcare aims to change the environment so that it is easier for patients to get good care, and for the health care workforce to provide it in a sustainable way.
Wendy Dean is the co-founder of Moral Injury of Healthcare and co-author of If I Betray These Words.

Like many in her age group, Jenny Li, a 38-year-old who works in retail planning, recently found herself serving as counselor and advisor to her parents, who were approaching age 65 and preparing to go on Medicare.
Like many in their age group, Li’s parents were not well versed on the program, but they had heard the ubiquitous sales pitches for Medicare Advantage. They were on the verge of signing up, unaware that the MA landscape is fraught with scams and deceptive sales practices designed to obfuscate and confuse.
Today a large number of seniors don’t know that only traditional Medicare allows you to go to any doctor at any time. Along with a supplemental policy called Medigap, this combination covers virtually all medical bills without the restrictions that come with MA plans. However, because of the federal government’s role in backing the growth of MA plans, as well as continuous promotion by the private health insurance industry itself, Medicare Advantage now accounts for more than half of the Medicare market.
Over the past several years, seniors have been encouraged to drop their traditional Medicare coverage in favor of MA plans. And for years, the government has overpaid the health plans, which enabled them to entice seniors with gym memberships, groceries, and some dental and vision care that traditional Medicare isn’t allowed to offer. In effect, the Medicare market is now the proverbial uneven playing field thanks to the federal government under the leadership of both Democrats and Republicans.
The complexities of one of the country’s few social insurance programs have bedeviled seniors since Medicare’s inception in 1965. From the beginning, the program has been plagued by scam artists with sales tactics designed to mislead, confuse and entrap seniors.
Li did not want her parents trapped in an Advantage plans provided by a profit-making insurance company. While it’s possible to return to traditional Medicare, there’s a catch: After you enroll in an MA plan, you can no longer buy a Medicare supplement policy without what’s called “underwriting,” a practice that means insurers will investigate your medical history and offer affordable coverage only to those in excellent health. In a few states, you might be able to get a supplement during certain times of the year, but the only states where you can buy a supplement anytime regardless of your health are Maine, Massachusetts, Connecticut and New York. Since Li's parents live in Pennsylvania, they wouldn’t have that escape. She decided to pay the monthly premium for supplement plans, which now cost $147 for her mom and $166 for her dad. At first, her mom resisted. Why would you pay for something that’s free, she argued? In their close-knit Chinese community they had heard a lot about MA plans that came with no premiums.
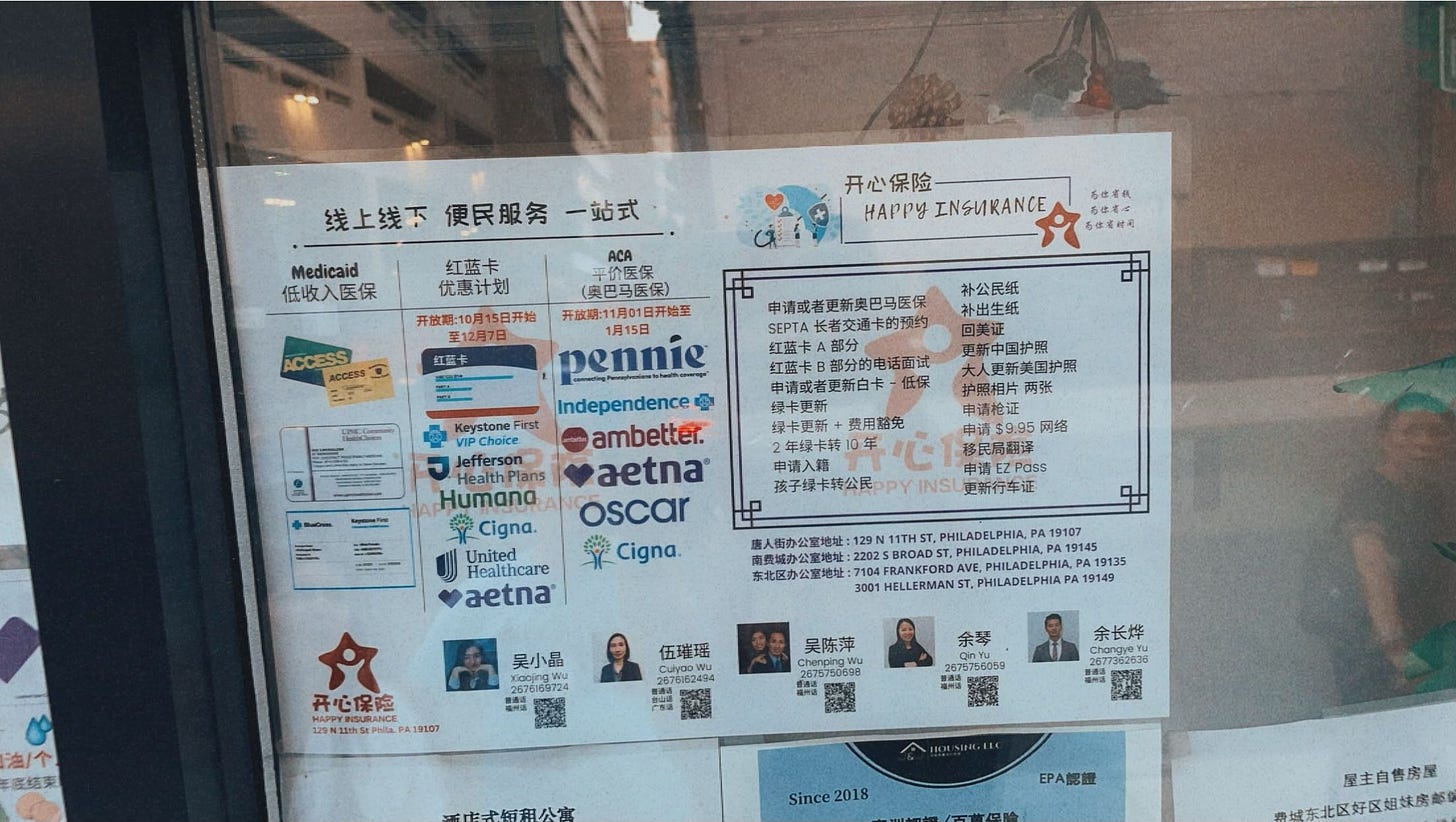
While MA sales pitches emphasize that in most cases there are no upfront premiums, the plans are not free. Those who sign up are likely to encounter high deductibles usually not discussed during sales presentations and not mentioned in TV promotions, especially if they seek care outside of their health plans' limited provider network.
To get a flavor of current out-of-pocket limits, I consulted the “Medicare and You Handbook” for New York City and found a Humana preferred provider plan for a New York City ZIP code with out-of-pocket limits ranging from $9,350 to $14,000. The limits for a UnitedHealthcare AARP Medicare Advantage PPO plan ranged from $8,900 to $14,000.
It wasn’t easy for Li to convince her parents not to sign up.
“I don’t think they knew it was Medicare Advantage. They thought it was part of Medicare,” Li said.
“When they became eligible for Medicare, it was a foreign system to them. Whatever they can save, they do. If they could buy something in the middle price range, that’s what they did. Medicare Advantage was the middle-of-the-road option for them. My mom was adamant this was Medicare.”
Li decided to pay the premiums on her parents’ supplement policies when she learned they could have trouble buying Medicare supplement policies later on.
That turned out to be a lucky decision. Four years after she bought the Medigap policies, her father required triple heart bypass surgery. “Everything was covered [under traditional Medicare],” Li said, except for deductibles of $1,872. “It was so easy.”
A few years ago I asked a St. Louis woman to keep track of what goodies her Medicare Advantage plan offered throughout the year. Her experience was instructive. She told me the promised benefits were pretty skimpy, and the dental benefit paid so little her husband ended up using a dental benefit that his former employer had provided. What do you want your insurance to do: pay for a necessary heart bypass, or give you a bag of gifts along with potential fights with an insurance company to pay for a major illness?
But sales pitches are persuasive. I once attended an insurance company sales event at a coffee shop. At the end of the program, one man refused to talk to me. He was in a hurry, he said, because he might lose his chance to sign up for a Medicare Advantage plan.
]]>
The pain Jennifer Braunagel endured during an eight-month battle with her insurance company over rheumatoid arthritis medication was physical. The insurer’s denial of the only drug that offered hope in fighting Braunagel’s chronic illness meant ongoing bouts of severe pain in her hands, back, ankles and other joints, as well as vision problems and difficulty breathing.
But the rejection, after countless calls and pleas to try the advanced infusion drug Actemra prescribed by her doctor, also wore her down emotionally.
“I have been in a flare just because of stress and being just so totally upset and floored that an insurance company can do this to you and can just push you to the side. Like I'm nobody. And I just don't get that,” Braunagel said.
Unfortunately, Braunagel’s gut-wrenching case is not unique. Although the health care debate in America often focuses on the uninsured, the reality is that millions who do have health insurance face problems when they try to use it – especially when approval is needed for increasingly expensive prescription drugs.
A 2023 survey by the health site KFF found that roughly six out of 10 patients reported an issue with an insurance claim – often during the process known as prior authorization, when an insurance company like Braunagel’s carrier, Aetna subsidiary Meritain Health, must approve a medical procedure or a new drug treatment ahead of time. The vast majority of patients whose requests for approval are rejected don’t file a formal appeal, either because they don’t understand their right to do so, don’t feel well enough to fight a denial, or just think it would be too time-consuming or futile to even try.
Braunagel’s problem may have been numbingly familiar, but her solution was a new high-tech approach that could offer hope to other U.S. patients who face insurance company gridlock.
After those months of frustrating calls and failed appeals, Braunagel and her doctor’s office turned to a startup company called Claimable that is using artificial intelligence, or AI, to rapidly write appeal letters meant to push the buttons that will get a big insurance company to change its mind. They used AI both to mine the most salient facts in Braunagel’s case and also to pull language from previous successful appeal letters.
In this case, it worked.
The appeal letter crafted by Claimable was also forwarded to the Department of Labor in Braunagel’s home state of Illinois, which took up her case and sparked action in just five days. Today, Braufagel’s every-four-week injection of Actemra – which would have cost $589 out-of-pocket – is covered, and the treatment is working.
“The AI is the mechanism, but this is really about helping people who have been marginalized,” said Warris Bokhari, the medical doctor who launched Claimable and serves as its CEO. Braunagel was lucky to have advocates like her suburban St. Louis arthritis clinic, he said, but most patients are outgunned by Big Insurance and lack the time to make appeals and the know-how to win. So, most don’t aggressively challenge a prior-authorization rejection, even when a medical procedure or a new treatment regimen could substantially improve their quality of life.
Cigna, where I was a vice president before I became an industry whistleblower, was the subject of a damning 2023 investigation by ProPublica that found a medical director who rejected 60,000 claims in just one month and who typically did not even read them. ProPublica found that just 0.1 percent of patients rejected under prior authorization tackled the appeal process an appeal.

But Braunagel, 52, a bus dispatcher and receptionist, is a fighter. She had already been fighting off breast cancer when her rheumatoid arthritis symptoms added a new complication to a series of ongoing health problems. She said the pain started in her hands and then spread. “It hurt to breathe,” she recalled. “My elbows, my legs. I was getting cramps, these awful cramps in the back of my leg that every time I moved my toes a different way…I would wake up in the middle of the night.”
The doctors treating Braunagel at the Arthritis Center in the St. Louis suburb of Bridgeton didn’t have much success with the initial medications, which is why they prescribed Actemra, an expensive infusion medicine that offered more promise. Meritain Health initially denied the Actemra request in favor of a less expensive type of medicine – a practice known as step therapy, in which a patient is asked to spend weeks or months on a less costly medicine that doctors fear won’t be as effective.
Julie Baak, the practice manager at the Arthritis Center, said 85% of her job is working on appeals like the Braunagel case, and it’s a source of great frustration for her.
“My 25-person support team – for one physician – exhausts the 'normal' insurance and [pharmacy benefit managers] channels, which work just as they are designed, to delay and deny patient care,” Baak said. “It takes 10 to 25 hours for me, an expert advocate, to work one case successfully.” That involves communicating with the patients and their employers, and even posting on popular social media sites like YouTube or TikTok to shame big insurance companies.
So neither Braunagel nor Baak’s team at the Arthritis Center were willing to take ‘no’ for an answer. The insurance company’s initial rejection touched off a flurry of phone calls and, over six months, two formal appeals and four separate letters of medical necessity requesting the more aggressive treatment. Meritain Health was not budging from its position, so Braunagel’s doctors took the novel step of asking Claimable to craft a new appeal.
Bokhari, who’d worked previously on the cutting edge of digital medicine, saw in the rapid advances of AI in the 2020s an opportunity to make the appeals of prior-authorization rejections go faster and – more importantly – with a better chance for success. Said Bokhari: “We’ve created a system that’s obsessed with protecting a payment model” – and not with solving the problems of patients.
It took Claimable less than a day to file an appeal using AI. Its letter said that Meritain Health had violated its own guidelines in recommending step therapy when it had already been shown to be inadequate and pointed out that Braunagel was entitled to a decision in just 72 hours. The new appeal was copied to company executives and to regulators, including the state labor official who intervened on Braunagel’s behalf.
“It took 30 minutes for Jennifer to tell her story to Claimable,” Bokhari recalled. “We tried to highlight the humanity and the social isolation,” as well as her physical symptoms and her failed attempts at using other medications. He said the state official who read the letter was “astounded” at the lack of support Braunagel was receiving from her insurer.
Once the insurer approved Actemra, the results for Braunagel were dramatic – just as her doctors had hoped.
”After my first [infusion], I guess I wasn't paying attention.” she recalled. “It was on a Friday and I was flip-flopping in bed, and I woke up and I was like, ‘Oh, my back's not hurting. Oh my gosh!’ It was the most amazing thing. That pain that I have had for – I don't even know how long – out of my back and the stiffness. And I felt good.”
Baak, who devotes so much of her working day to insurance claims and appeals, sees enormous potential in Claimable’s ability to streamline the process. She praised it as a way to give “physicians the time to focus on what they are trained to do – get the right patient on the right drug.”
Remarkably, Meritain sent another letter to Braunagel this summer, telling her it had not received the medical reports it needed to continue approving her treatment, but this time the hold-up was temporary and her infusions every four weeks resumed. Although stress – like the kind from dealing with insurance companies – still triggers occasional arthritis flares, Braunagel said she’s been able to visit her three grandchildren in San Diego, with plans to return in a few weeks.
Braunagel was shaken by her experience with her insurer and wonders how older patients can deal with all the roadblocks. “This country is supposed to be the greatest country in the world,” she said, “and people are suffering because of these insurance companies.”
]]>
Today, as we honor the brave men and women who have served in our nation’s military, it is important to understand how they’re all too often being ill-served by the very institutions meant to support them. The U.S. Department of Veterans Affairs (VA), historically a beacon of care for millions of veterans, has increasingly been required to shift services to private health insurance giants like Cigna, Humana, and UnitedHealth Group and the health plans and pharmacy benefit managers they own and operate. This creeping privatization isn’t just symbolic — it’s impacting veterans’ health outcomes, quality of care, and the VA’s financial stability and is at the heart of many veterans’ complaints about the VA.
What we’re seeing is a slow but steady transformation, in which Big Insurance is stepping in to “supplement” VA care. But in reality, this often means veterans are being pushed into a fragmented, confusing system run by corporations that are more interested in boosting their bottom lines than providing access to quality care. For example, veterans referred outside the VA system to private insurers’ provider networks now face complex billing structures, skyrocketing out-of-pocket costs, and restrictions that make it hard for them to get the care they need.
This is nothing new with these companies. Those insured in the civilian health insurance market are increasingly having to contend with the burden of prior authorizations, denied claims and steep annual premium and out-of-pocket increases that have become standard with private coverage.
In a troubling trend, privatized VA care often includes narrow provider networks that restrict veterans’ access to specialists and therapies they need. Many vets find that they have to travel far from home or wait weeks for treatment — putting their health and well-being at risk. For veterans struggling with chronic conditions, mental health needs, or combat injuries, this lack of accessible, high-quality care can be devastating.
Studies show that veterans receive higher-quality care within the VA system than through the private sector. Yet, as funding flows from taxpayers to Big Insurance, it’s clear the mission has shifted away from what’s best for veterans. Veterans’ care should not be outsourced to companies that prioritize shareholders over patients. We should be strengthening the VA system, not hollowing it out in the name of "efficiency" or cost-cutting measures that ultimately cost us far more in terms of veterans' health and taxpayers’ money.
This Veterans Day, let’s remember that our nation’s commitment to those who served must extend beyond words. We owe it to our veterans to provide them with a VA system that delivers the care they need and deserve and that is not encumbered by profit-focused insurance corporations. The health of our veterans, and indeed the strength of our nation, depends on it.
]]>
A new study published in Health Affairs—“High-Deductible Health Insurance May Exacerbate Racial And Ethnic Wealth Disparities” by Naomi Zewde, Sergio Rivera Rodriguez, and Sherry A. Glied — exposes how high-deductible health plans (HDHPs) compound racial and ethnic wealth disparities in America, effectively making health care less available and affordable for Black and Hispanic families.
Even when I still worked in the industry, research showed that the burdens of out-of-pocket medical expenses — deductibles, copayments and coinsurance — fall hardest on low-income households, especially among Black and Hispanic families. Nearly 20 years ago, I recall sitting in a leadership meeting at Cigna. The company’s newest VP, who had made a name for himself in the so-called “consumerism” movement, tried to convince us that moving more Americans into high-deductible plans would work in the everybody’s interests. We could easily see how they would benefit Cigna and other insurance companies, but we couldn’t figure out how patients would benefit. We peppered him with questions, and his answers were not landing. He eventually said, "Look, you're just going to have to drink the Kool-Aid." Most of us did and most are still drinking it. I remained a skeptic. The Health Affairs study gives us a deep glimpse into what all of us in that meeting knew would happen even if we weren’t willing to acknowledge it: HDHPs would widen the wealth gap and exacerbate health inequities in this country.
The authors examined data on privately insured families from 2011 to 2018 and found stark wealth disparities between racial and ethnic groups, even when families had similar incomes. White families with private insurance, on average, had more financial assets across all income levels than their Black and Hispanic counterparts. In the lowest income bracket, White families had over 350% more financial assets than Black families.
In this way, high deductible plans — which require enrollees to shoulder significant costs upfront before insurance coverage kicks in — aren’t just financially burdensome. They reinforce a system in which financial stability and access to necessary care are out of reach for many Black and Hispanic families. The median financial assets for low-income Black and Hispanic families enrolled in HDHPs were around $2,200 and $2,000, respectively — far below the typical deductible for family coverage, which averages about $5,000. For these families, covering medical expenses under such a HDHP means draining any modest savings, leaving them economically vulnerable.
HDHPs emerged in the 2000s, incentivized by the Medicare Modernization Act, which introduced tax-favored Health Savings Accounts (HSAs). These accounts, available only to those in HDHPs, were initially intended to encourage consumers to spend more thoughtfully on their health care. However, HSAs disproportionately favor higher-income, wealthier, and largely White households that are more likely to have financial assets to set aside in any kind of savings account. Lower-income Black and Hispanic families, on the other hand, are left to manage HDHPs without the financial buffer an HSA provides wealthier families, amplifying the financial precarity they face.
The researchers make it clear that HDHPs have created a two-tier system within the privately insured population. Wealthier White families, many already advantaged by generational wealth and financial security, have the resources to manage high deductibles and to benefit from HSAs. Meanwhile, Black and Hispanic families with HDHPs face the dual burden of health costs and limited wealth, translating into significant disparities in health care access.
The study’s findings underscore a critical, often overlooked dimension of health care inequality: wealth. Historically rooted racial wealth gaps persist because wealth is not merely a function of current income but rather of generational accumulation—or lack thereof. The gap between White families and Black or Hispanic families reflects hundreds of years of exclusionary policies, from redlining to disparities in educational and economic opportunities.
HDHPs exacerbate this issue by turning health care affordability into a question of wealth. When American families with fewer monetary reserves have to tap into already limited savings to pay for medical care under HDHPs, they are left even more financially vulnerable. The result? Health insurance that was supposed to protect families instead deepens racial inequities and make many families even poorer.
The study’s findings highlight a pathway for policymakers aiming to create a more equitable health care system. Potential reforms could include capping deductibles in HDHPs or limiting the tax benefits of HSAs to reduce the wealth advantage they provide to affluent families. Policymakers could also explore expanding programs that reduce out-of-pocket costs for low- and moderate-income people. Such measures could help prevent wealth from becoming a barrier to accessing necessary medical care.
The report from Health Affairs is a stark reminder that health care policies do not exist in a vacuum. High-deductible health plans may be marketed by insurers as an effective cost-sharing solution, but they come at a significant cost for the economic stability and health of American families. Addressing these issues is a matter of urgency, as our health care system cannot truly be equitable if access to care depends on the financial assets a family can draw on in times of need.
This study is a call to action for policymakers to reconsider how our insurance system disproportionately harms families of color. The path forward requires dismantling policies that deepen inequality and moving toward a health care model that truly serves all.
]]>
Tuesday’s election will have significant consequences on what health care issues lawmakers in Washington address after the first of the year – and how they will go about it – but it will not have much influence on the issues we at HEALTH CARE un-covered focus on.
I started this newsletter to raise awareness of how the industry that paid me well for two decades – the health insurance industry – really operates. With every story, we endeavor to pull the curtains back a little more, and that will not change. Big Insurance is an industry of middlemen that has grown to massive size and has become incredibly adept at fleecing both our government and our employers and that has erected barriers that make it increasingly difficult for Americans to get the care they need and at a price they can afford. Those barriers are there for a purpose: to make it less likely insurers will have to pay for medically necessary care so that more money is available to reward shareholders, including the occupants of the companies’ C-suites.
As we go forward, we will continue to report on what that fleecing looks like, how big it is, and how much it costs us as taxpayers, employees, retirees and patients. And we will continue to report on the consequences of those barriers, namely:
outrageously high out-of-pocket requirements;
excessive and unnecessary prior authorization requirements; and
inadequate and often poorly constructed and self-serving provider networks.
By the way, those outrageously high out-of-pocket requirements imposed by Big Insurance are among the reasons Americans are increasingly having trouble putting food on the table and paying the rent. Exit polls I’ve seen showed that around 65% of voters said their main concern was the economy and inflation. The New York Times, in a piece explaining how the Democrats fell so short in races across the country and from the top to the bottom of the ballot, noted that being able to pay the rent was far more of an imperative to working-class voters than pledges to save democracy. Politicians would be smart to do something voters can experience personally, like getting relief from exorbitant deductibles and other out-of-pocket requirements that have put 100 million Americans into medical debt. Voters do not have the ability to vote Cigna and Aetna and UnitedHealthcare out of their lives, but they can vote politicians out of office. And they just did.
While we at HEALTH Care un-covered will continue to focus on what happens or doesn’t happen in Washington and state capitals, we will also continue to focus on what is going on in the private sector – the marketplace – that is promising, that can save both our employers and the rest of us billions of dollars while also making it easier for patients to get the care they need from high-quality health care providers without sinking deep into medical debt.
I’m proud of the fact that our stories have helped educate lawmakers on both sides of the political divide (as well as employers, advocates, agents and brokers, the media and consumers). We are now seeing real bipartisan support for incremental but extremely important reforms, including legislation that would reduce if not eliminate those industry barriers and make it easier for patients to overcome them. I’m encouraged that Republicans and Democrats alike are cosponsors of legislation to reform the prior authorization process, to force pharmacy benefit managers to change their business practices and operate more transparently, and that would reduce the maximum out-of-pocket requirements for all of us, especially for low- and moderate-income Americans and people with chronic conditions.
I’m also seeing bipartisan support for efforts to reduce the massive overpayments to insurers that sell Medicare Advantage plans, although Wall Street seems to think the next Trump administration will turn the other way and allow the profiteering to continue. Yesterday, the share price of the big insurers that dominate the MA market rose significantly. We’ll see if Republicans who are true fiscal watchdogs will give Big Insurance the big pass investors are expecting. I’m pretty confident that at least some and maybe many Republicans in Congress will join Democrats in demanding more accountability in the MA program.
Speaking of investors, the big insurer whose stock price went south after the election was Cigna, which announced plans last year to get out of the Medicare Advantage business. Cigna is now predominantly a PBM: Its Express Scripts business is far bigger and more profitable than the health insurance side of the company, and it no longer has an MA book of business. You can be certain that the results of Tuesday’s election will make it more likely that Cigna will once again consider buying Humana, the second-biggest MA player.
But as regular readers know, we are not focused exclusively on what’s happening in Washington. Far from it. There is a tremendous amount of disruption occurring in the private sector that has the promise of being more of a headache to Big Insurance than lawmakers in DC or elsewhere. That’s why we launched the “Disintermediation” beat. You’ll be seeing many more stories about health care business leaders and entrepreneurs who are making substantial headway in eliminating the middlemen that add little if any value but enormous cost to the U.S. health care system. We have several profiles and Q&As with these disruptors in the pipeline. So stay tuned.
A final note: I’m grateful for and proud of the diversity of our readership. Our thousands of subscribers span the ideological spectrum, which is remarkable in this day and age. You often disagree – and don’t hold back when you do – but, for the most part, you behave civilly and respect each other’s point of view. We have become a broad-based community of individuals who care about the health and well-being of our fellow Americans and who genuinely want to be a part of the solution. So thank you – especially to those of you who have become paid subscribers, even though all of our content is free.
]]>
With the election looming and the beginning of annual open enrollment periods for health insurance plans, it is vital to pull back the curtain on the influx of money from Big Insurance corporations to political campaigns and lobbying.
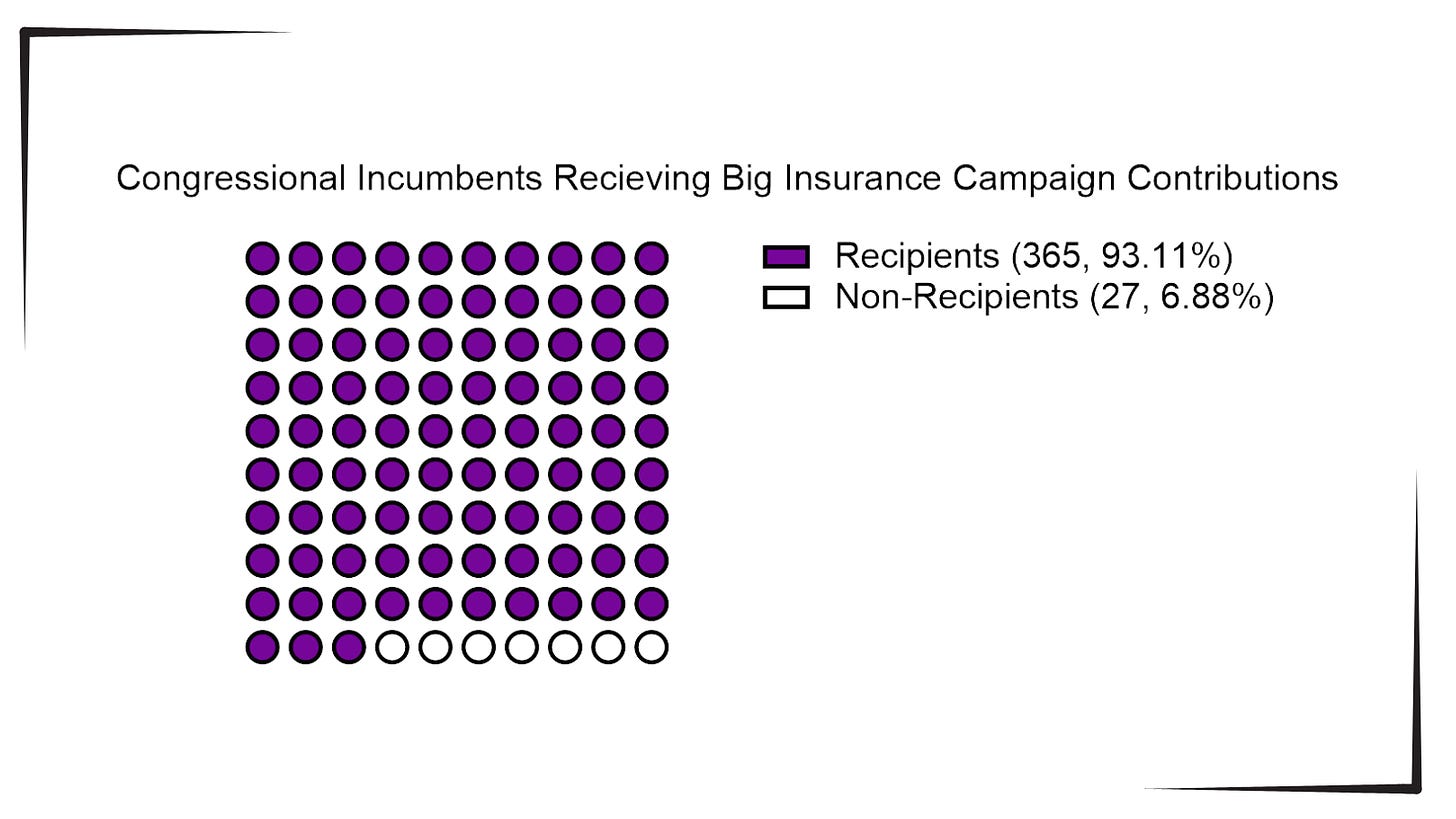
Data available from OpenSecrets.com thus far in 2024 shows that 93% of Congressional incumbents running in 2024 received contributions from Big Insurance, including 100% of Senate incumbents. These insurance corporations run the ten largest Medicare Advantage plans in the country and are known to deny needed health care and defraud the government, but face little to no consequences.
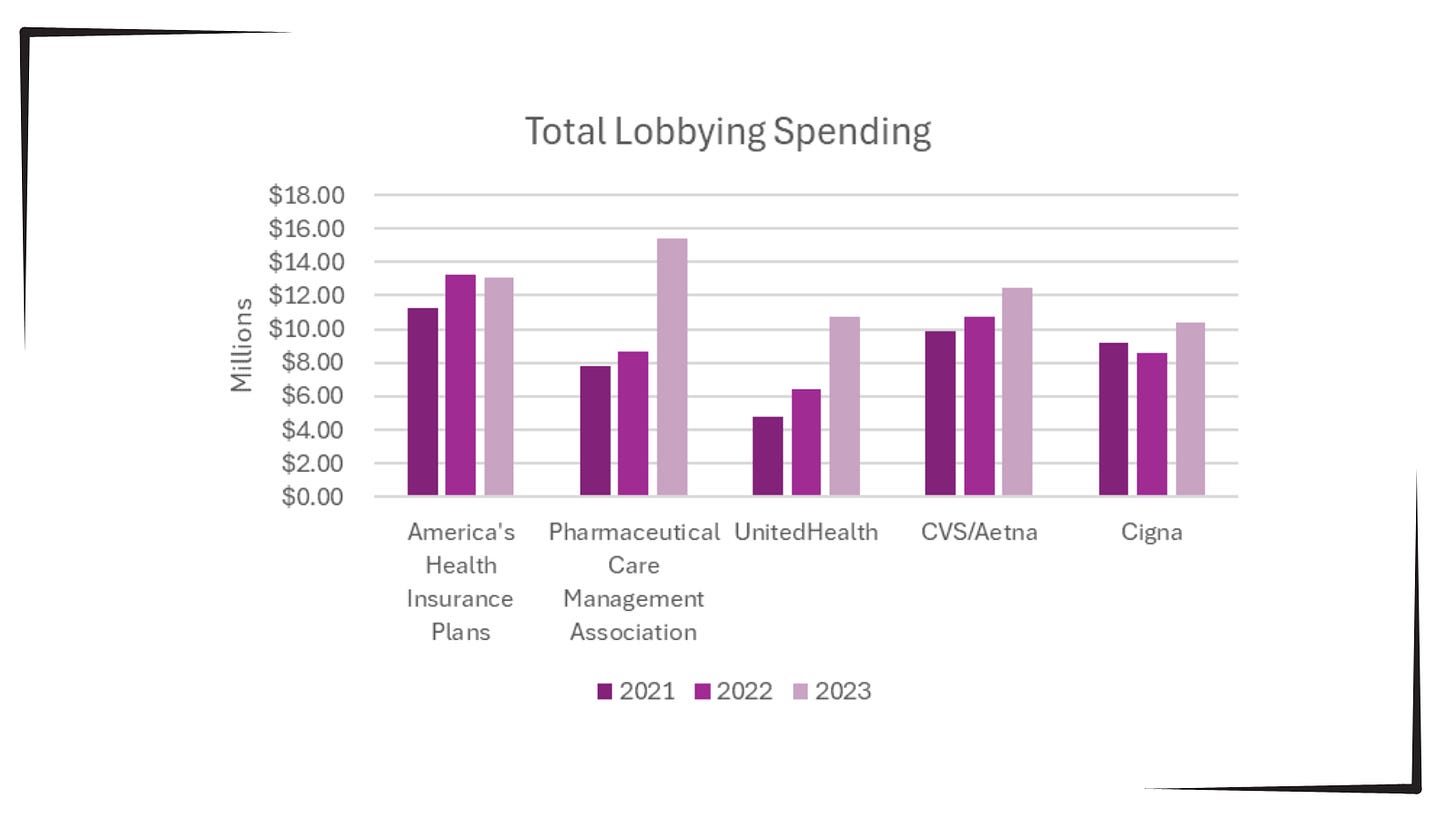
Additionally, as bipartisan scrutiny of pharmacy benefit managers (PBMs) and Medicare Advantage plans has intensified, spending by Big Insurance on lobbying has increased.
This open enrollment season, people struggling to choose a health insurance plan that they can afford and that provides the care they need may ask themselves, “Why is our health care system like this?” The immense amounts of money Big Insurance spends to blanket members of Congress with contributions and lobbying hold the answer.
Additional analysis following the election will allow evaluation of just how much Big Insurance spends on politics to help protect industry profits and will give health reform advocates an idea of how to overcome this influence to pass policies for patients, not profits.
]]>
Health columnist and former editor of Modern Healthcare Merrill Goozner has sounded the alarm about what might happen to the U.S. health system if Donald Trump gets to the White House. Indeed he writes in GoozNews, his Substack column, “The stakes for health care: The fate of America’s inadequate, unaffordable and unequal health care system is on the ballot. Harris gives us a chance to make it better. A Trump victory guarantees something worse.” I have known Goozner for a long time, and can say he knows the system very well. His worries are well-founded, and those who are concerned about losing their health care or finding it severely cut in a Trump presidency should read his column.
Despite the significant gains in insurance coverage made by the Affordable Care Act in the last 11 years, the American health care system is still in need of serious repair.
“Most people don’t know or are dimly aware” that Harris has proposed the most significant Medicare expansion since adding a prescription drug benefit in 2003,” Goozner wrote. Her plan “would be wildly popular if more people knew about it.”
A second Trump presidency “will result in millions of people losing their health insurance coverage or seeing their benefits sharply reduced,” he wrote.
Goozner also promoted Harris’ plan to add a home-care benefit to Medicare which would offer financing for in-home aides to help infirm and elderly family members struggling to stay out of nursing homes. He notes that 75% of U.S. adults support a program to help pay for long-term care, and cites the programs other countries such as Japan have had for some time now. In 1993 I was in Japan as a Fulbright scholar studying the Japanese health system, and was amazed at the long-term care program the country already had enacted. Thirty-one years later, the U.S. is still not even talking about creating such a program although Goozner reports that 75% of adults in the U.S. support that effort.
Project 2025, the conservative Heritage Foundation’s policy plan designed to guide a second Trump presidency, calls for Medicare Advantage for all, which would take away the more comprehensive coverage of traditional Medicare and a supplement coverage that millions of Americans still have and want.
As I wrote earlier this year, “The seeds of Medicare’s destruction are in the air. The program as it was set out in 1965 has kept millions of Americans out of medical poverty for over 50 years, but may well become something else – a privatized health care system for the oldest citizens whose medical care will depend on the profit goals of a handful of private insurers.”
]]>
As my colleague Joey Rettino wrote earlier this week, health insurance companies’ provider networks are plagued with ghosts, especially when it comes to mental and behavioral health. Numerous studies have shown that in many cases, more than half of the providers listed are not seeing new patients or are no longer in the insurers’ networks. But patients aren’t the only ones getting the short end of the stick from companies like UnitedHealthcare. The country’s mental health providers are getting shafted, too.
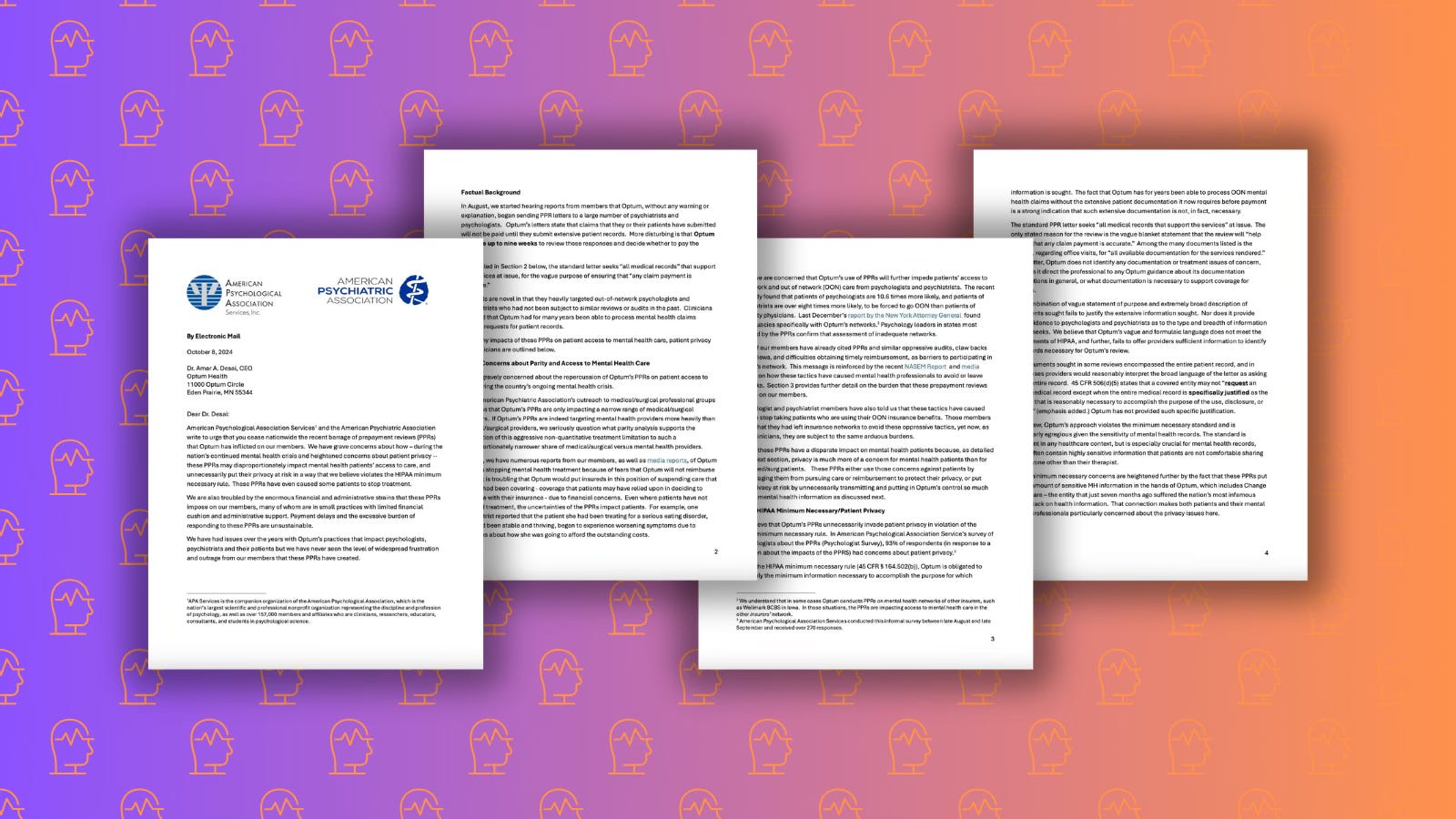
According to a complaint first published on ClearHealthCosts by Jeanne Pinder, The American Psychological Association and the American Psychiatric Association wrote in a letter to Dr. Amar A. Desai, CEO of UnitedHealth Group’s Optum Health, that Optum’s pre-payment reviews (PPRs) are "unsustainable," and that the “enormous financial and administrative strains" are driving some clinicians to stop accepting insurance altogether.
PPRs are a process in which health insurers or their vendors or sister companies, like UnitedHealthGroup’s Optum, require physician practices to submit extensive documentation — such as medical records and treatment notes — before they’ll pay claims for services rendered. For clinicians, this adds administrative burdens and payment delays.
Small practices with limited financial and administrative resources are especially vulnerable. Instead of being able to focus on caring for patients, they’re drowning in paperwork, waiting months to be paid, if at all. The joint letter reads:
American Psychological Association Services and the American Psychiatric Association write to urge that you cease nationwide the recent barrage of prepayment reviews (PPRs) that Optum has inflicted on our members. We have grave concerns about how – during the nation’s continued mental health crisis and heightened concerns about patient privacy – these PPRs may disproportionately impact mental health patients’ access to care, and unnecessarily put their privacy at risk in a way that we believe violates the HIPAA minimum necessary rule. These PPRs have even caused some patients to stop treatment.
The financial strain is so severe that 44% of psychologists surveyed said these delays threaten their solvency. This is not just a minor inconvenience — it's a direct attack on mental health care delivery at a time when the nation is in the grips of a mental health crisis.
This bureaucratic hurdle is another way UnitedHealth and other Big Insurance corporations are violating the Mental Health Parity and Addiction Equity Act, which requires them to treat mental health care the same as physical health care. UnitedHealth knows this is the result of PPRs, in fact they are happy with this result because it keeps them from having to actually pay for their customers’ care.
UnitedHealth Group, via Optum, is making it nearly impossible for clinicians to keep their doors open and serve their patients. As Pinder points out, patients are pausing or stopping treatment because of these delays. When clinicians are forced to navigate Optum’s labyrinthine reviews instead of focusing on their patients’ care, everyone loses.
]]>
As the Medicare open enrollment period continues, Democratic leaders of the Senate Finance Committee, House Energy and Commerce Committee, and the House Ways and Means Committee sent a letter today to the Centers for Medicare and Medicaid Services illustrating how privatized Medicare Advantage (MA) plans are “failing to deliver” for seniors and people with disabilities. The letter specifically mentions the delays and denials of care using prior authorization, the “bait and switch” in marketing MA plans, and the misaligned incentives for brokers to promote only some MA plans. This letter is a significant development in the continued scrutiny of Big Insurance companies that run MA plans because it signals a shared focus on MA and alignment on necessary reforms from the top three Democratic members of Congress with jurisdiction over this issue.
Chair Ron Wyden and Ranking Members Frank Pallone and Richard Neal suggest reforms to the prior authorization process in MA that have potential to decrease delays and denials of care. They suggest making data on the use of artificial intelligence (AI) and algorithms in coverage decisions public, including the denial and appeal rates and types of care that are being denied. This would certainly help in understanding the extent of the malignancy that is care denials. Current research on this issue is limited by data availability so it is likely we do not even know the full extent to which Big Insurance is refusing care to seniors and people with disabilities on MA.
The members of Congress also recommend that MA plans disclose the methodology behind the AI tools and algorithms they use to review prior authorizations. This is a key recommendation because physicians and other medical professionals have reported that when they try to gather information on why the insurer’s algorithm denied their patient’s care they are told “that's proprietary.” When Big Insurance withholds the methodology behind their AI tools making coverage decisions ensures that doctors and patients have no recourse to fight care denials and makes it harder for patients to get care.
These actions by insurance corporations also likely violate the law which states that MA plans must use utilization management guidelines that “are developed in consultation with contracting physicians” and that the guidelines “are communicated to providers.” The recommendation by Ron Wyden and Frank Pallone and Richard Neal for transparency in AI used in MA is vital, and likely supported by existing law and regulation.
The letter also recommends ensuring that MA network directories accurately list providers within the network to enable people to determine if the plan has the medical providers they require for their care. As health insurance companies become more complex and opaque, it is increasingly difficult to find a provider in network for medical care.
Further, Big Insurance puts the burden of determining if a doctor is really in network by adding disclaimers to their website and phone recordings claiming “This information is subject to change at any time. Please check with the provider before scheduling your appointment or receiving services to confirm he or she is participating in your health plan’s network.”
If a patient receives services from a doctor listed on their insurance plan’s network, but the information is out of date, the insurer can deny the claim stating that the provider is out-of-network and cite the disclaimer as a way to avoid paying for services. For all the talk from Big Insurance that they can administer health coverage more efficiently than other entities, it makes sense to make them do the work to ensure their directories are accurate and honor visits to any medical provider that was listed in network at the time the appointment was made, even if that information was incorrect on the insurer’s network directory.
Finally, the letter’s authors recommend detailed reporting of how insurance companies and subcontractors are spending money on marketing and broker’s commissions. They also suggest increasing funding for public State Health Insurance Assistance Programs (SHIPs) which provide unbiased assistance to enrollees in choosing their Medicare plan. These reforms would be a big step towards avoiding the misaligned incentives for brokers to steer people into certain MA plans that provide the best commissions, without regard for the quality of care that MA plan provides.
A further step that would provide even more education and support for beneficiaries in choosing their Medicare plan would be to prohibit the use of taxpayer dollars on marketing and brokers by MA insurers. Instead, the $6 billion that Big Insurance currently pays for these services and those incessant commercials about their MA plans could be re-routed to SHIPs to increase their capacity to provide resources and advice on how to choose the best Medicare benefits.
The letter from Chair Wyden and Ranking Members Pallone and Neal places focus on important issues in MA and charts a path for potential reform in the next Congress. The recommendations in the letter demonstrate that the leaders of key Congressional committees understand the dangers of MA and what needs to be done to curb them. In addition to the recommendations in the letter, action to stop the $140 billion per year in overpayments going to Big Insurance running MA plans would complement this set of reforms perfectly and protect Medicare for decades to come.
]]>
This Halloween, as you prepare for haunted houses and spooky stories, let me tell you about a specter that doesn’t just lurk on October 31 – but instead every day of the year for far too many Americans. I’m talking about the ghost network lurking inside your health insurance plan.
Many health insurance provider directories — whether public or private — are filled with outdated or inaccurate information, giving you the illusion that help is just a phone call away. But when you finally reach out, it very well could be a doctor or therapist who has retired, moved away or simply isn’t taking new patients anymore. It’s a cruel trick, and for millions of Americans struggling with mental health issues, there’s no treat in sight.
Directories claim to offer a wide range of in-network mental health professionals, but in reality, many of these providers are unreachable. A Senate Finance Committee study revealed that of 120 mental health provider listings across 12 Medicare Advantage plans, only 18% of the listed providers were available for appointments.
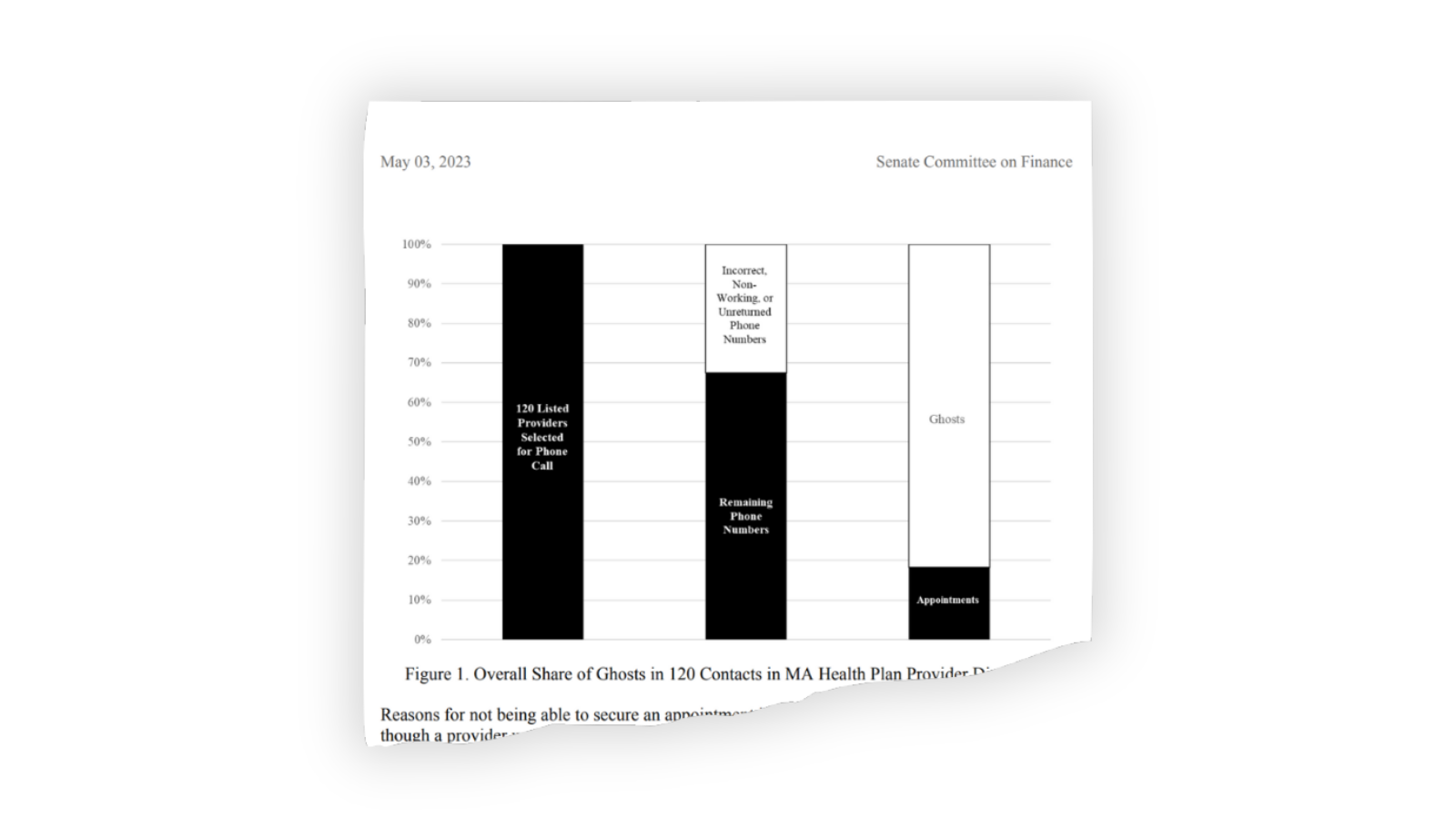
Even worse, a similar study by the Seattle Times found that only 8% – yes, 8% – of the 400 mental health providers listed by Washington state’s largest insurers offered appointments. If this sounds like a horror movie, that’s because it is — except this is no movie, and the real-life consequences are devastating.
Why do these ghost networks exist? The simple answer: profits.
Health insurers benefit from creating the illusion of a robust, in-network mental health provider base while avoiding the costs associated with actually providing access to care and paying for it. When people can’t find an in-network provider, many either give up on seeking care entirely or go out-of-network, often facing significantly higher costs. Either way, insurers save money by paying fewer claims. The deliberate creation of ghost networks ensures that patients, already grappling with mental health challenges, are more likely to get lost in this haunted maze of false promises while insurers cash in their premiums.
The consequences of these ghost networks are staggering. According to Harvard Law’s Bill of Health, more than half of adults experiencing a mental illness in the U.S. — more than 28 million people — go without treatment. Ghost networks only deepen this crisis by adding unnecessary barriers to care. Patients are left with few options: They either wait endlessly for an in-network appointment that may never come, or they go out of network and bear the brunt of higher costs, which can be financially crippling. Many people simply give up, unable to afford the care they need, further exacerbating mental health issues.
So, what can be done to exorcise these ghost networks from our health care system?
Some lawmakers are starting to act. The federal No Surprises Act, passed in 2021, mandates that health insurers update their provider directories at least every 90 days. While this is a step in the right direction, compliance has been weak due to a lack of enforcement and inadequate staffing on the part of insurers. Additionally, the Consolidated Appropriations Act of 2023 requires Medicaid plans to maintain accurate and searchable provider directories, but enforcement remains limited. And neither law allows patients to take insurers to court if they fail to maintain accurate directories.
More promising legislation could be on the horizon, however. The Behavioral Health Network and Directory Improvement Act, sponsored by Sens. Tina Smith (D-Minnesota) and Ron Wyden (D-Oregon) would enforce stricter directory adequacy standards, require insurers and the federal government to conduct audits on the accuracy of provider networks, and publicly share their findings.
States also have a critical role to play, and many already have network adequacy standards that require insurers to maintain a certain number of in-network mental health providers who are geographically accessible.
Ultimately, insurers need to do more than just comply with regulations; they need to tackle the root causes of ghost networks. Notoriously low reimbursement rates for mental health providers are one of the biggest factors contributing to the scarcity of in-network professionals. Many mental health providers can earn two to three times more by charging patients out-of-pocket than they would by accepting Medicare or Medicaid. By increasing reimbursement rates, insurers could incentivize more mental health providers to join their networks, which would make ghost entries less common and increase access to care.
So this Halloween, as you carve pumpkins and don your costumes, remember that the real terror may not come from the ghosts hanging on your porch, but from the ghost networks hidden in your insurance plan. These networks are the ultimate trick, making it hard to treat your mental health care.
]]>
The Department of Health and Human Services' latest report on Medicare Part D provides encouraging news for millions of Americans who rely on prescription drugs. Thanks to the Inflation Reduction Act (IRA), proposed by the Biden-Harris administration and passed by Congress in 2022, nearly 1.5 million Medicare beneficiaries saved close to $1 billion in out-of-pocket drug costs during the first half of 2024. This is a significant milestone in reducing the financial burden of uncovered medical expenses for America’s seniors and people with disabilities.
For too long, Medicare enrollees had no limit on their out-of-pocket costs, leaving many vulnerable to devastating financial consequences, especially those who rely on life-saving medications. Before the IRA, some enrollees faced drug costs as high as $60,000 a year.
This year marked the first-ever cap on those out-of-pocket costs, and the results have been transformative for many Americans even in just the first six months. The law’s current cap of $3,500 on out-of-pocket drug costs will drop even lower, to $2,000 next year, further alleviating the financial pressures on Medicare beneficiaries.
What’s especially promising is that this cap isn’t just benefiting a few; it’s bringing widespread relief. If the $2,000 cap had been in place for 2024, about 4.6 million people would have hit that limit by mid-year and would have faced no additional costs for the rest of the year. This is real, tangible change for millions of seniors.
For those grappling with chronic conditions like cancer, the savings are even more profound. A study published in September by JAMA found that the out-of-pocket cap saved cancer patients $7,000. Some of the most vulnerable populations — American Indian, Alaska Native and African American enrollees — have especially benefited from the cap.
The administration’s ongoing efforts to reduce drug costs include negotiating directly with pharmaceutical companies, allowing Medicare to leverage its bargaining power to secure lower prices for the most commonly used and most expensive drugs. The first round of negotiations is already producing savings, with prices expected to drop by as much as 79% for some medications starting in 2026. And for those with diabetes, the law’s $35 monthly cap on insulin costs offers a lifeline for millions of Americans who have struggled to afford this essential medication.
As we look ahead to 2025 and beyond, one thing is certain: The days of unlimited out-of-pocket costs for Medicare enrollees are behind us, but only for prescription medications. Congress and the next administration must push for an overall cap for people enrolled in traditional Medicare. Because of the lack of an overall cap, a stay in the hospital or extensive outpatient care can bury Medicare beneficiaries under a mountain of debt if they do not have a Medicare supplement policy to cover out-of-pocket obligations.
The lack of such a cap is a reason why many seniors are enticed to enroll in so-called Medicare Advantage plans despite their many unadvertised shortcomings, which we have detailed many times in this newsletter. And that $2,000-a-year cap on prescription drugs should apply to everybody, not just Medicare beneficiaries, as President Biden proposed in his State of the Union address earlier this year. Note: I run a coalition of organizations called Lower Out-of-Pockets NOW (LOOP NOW) that supports extending the $2,000-a-year cap for all Americans.
No one in the richest country on the planet should have to choose between their health and their financial well-being.
]]>
A recent Barron’s exposé detailing pharmacy benefit managers' (PBMs) backroom dealings in the opioid crisis should be read by everyone. PBMs, which most Americans encounter only indirectly through their health insurance plans, have quietly amassed enormous power over which medications we have access to — and how much they cost. This power extends not only to routine prescriptions but also, as it turns out, to some of the most devastating public health crises of our time.
The report reveals that the largest PBMs — CVS Caremark, UnitedHealth’s Optum Rx, and Cigna’s Express Scripts — were heavily involved in the distribution of OxyContin, a drug at the center of the opioid epidemic. Between 2016 and 2017, these companies raked in more than $400 million in fees and rebates from Purdue Pharma, OxyContin’s manufacturer. That these rebates were essentially tied to the volume of opioids sold is not just alarming — it’s emblematic of how these middlemen prioritize profit over public health.
The role of PBMs in drug pricing and availability has been contentious for years. The middlemen argue that their rebate system helps lower costs for employers and insurance plans, but this claim often falls apart under scrutiny. As Barron’s found, PBMs received as much as 19.75% in rebates from OxyContin sales, depending on the dosage and the number of pills prescribed. The higher the dosage, the bigger the rebate and profits. This system, which rewards higher utilization of a dangerous opioid, contradicts the PBMs’ – like CVS Caremark’s – own professed claims of fighting opioid abuse.
For years, PBMs have presented themselves as crucial gatekeepers, using their clout to negotiate lower drug prices. But the reality, as the article highlights, is far murkier. PBMs, including CVS Caremark and Express Scripts, claim they pass the majority of rebates back to their clients — figures as high as 99%. Yet, these rebates are negotiated in secret, and consumers rarely see the benefits. The rebates often serve to maintain PBMs’ relationships with drugmakers, who want to secure prime placement on formularies — the list of drugs an insurance plan covers.
The opioid crisis, as Barron’s demonstrates, could be a chilling preview of how PBM-driven rebate schemes might contribute to other drug pricing scandals. If PBMs have been willing to accept massive rebates from Purdue Pharma in exchange for keeping OxyContin widely available during a deadly opioid epidemic, what other drugs have been pushed to the forefront based on financial incentives rather than medical necessity or effectiveness?
The documents that Barron’s obtained, many of which were previously confidential, show that PBMs had ample opportunity to stem the tide of opioid overprescribing. They could have placed stricter limitations on OxyContin or required prior authorization (which they make significant use of for medically necessary medications) to ensure that the drug was being prescribed appropriately. Instead, they allowed Purdue to maintain a stronghold on the market. According to memos, PBMs even demanded higher rebates as the opioid epidemic worsened.
As the article suggests, this isn’t merely a historical issue. The opioid crisis may have peaked in the late 2010s, but its effects are still being felt today. And the practices of PBMs — opaque rebate deals, backroom negotiations and a relentless focus on profit — are still very much in place. While Purdue Pharma and its executives have been held accountable through legal settlements, PBMs have largely escaped similar consequences. The lawsuits against PBMs for their role in the opioid crisis are still ongoing, and CVS Caremark’s $5 billion settlement, finalized last year, didn’t even require an admission of wrongdoing.
This begs a larger question about the pharmaceutical supply chain as a whole. If PBMs have the power to negotiate how drugs like OxyContin are covered, and if their decisions are driven by maximizing profits through rebates, can they really claim to be stewards of affordable health care? (Regular readers of this newsletter should roll their eyes at that question.)
For too long, PBMs have operated with little transparency. As the Barron’s investigation shows, this secrecy has allowed them to profit handsomely from one of the deadliest public health crises in U.S. history. The opioid crisis could be the most egregious example of PBM malfeasance, but it’s far from the only one. As long as PBMs continue to operate without appropriate oversight, the American public will remain vulnerable to their influence over drug prices — and, by extension, their health.
]]>
Every day in America, thousands of patients get notices from their health insurers that the treatments their doctors say they need will not be covered because it is not, in the opinion of the insurance company, “medically necessary.” What they likely don’t realize, as a new expose by ProPublica and Capitol Forum shows, is that the medical necessity decisions often were not made by their insurers themselves but were outsourced to companies like Cigna’s EviCore, a major player in the "denials for dollars" industry.
EviCore generates profits for Cigna and its other customers by reducing access to medical care through a process called prior authorization, in which doctors must seek approval from EviCore before treating their patients. The reporters contend that EviCore’s business model revolves around denying care, a practice that not only jeopardizes patient health but also fattened its — and Cigna’s — bottom line.
At the heart of EviCore's system is an algorithm nicknamed “the dial,” which assesses whether a patient’s treatment should be covered and that can be manipulated to increase the number of denials. It’s all about where the threshold is set: If EviCore decides to boost its denial rate, it simply raises the bar and sends more cases to its in-house doctors for manual review. These reviews are no guarantee of approval, either. The investigation revealed that EviCore’s profit motive often leads to doctors being overruled by an AI system programmed not for patient care but for cost-cutting. The reporters say former employees confirmed that EviCore executives would tweak the system when the company wasn’t generating enough “savings” for its clients—savings that come directly at the expense of patients’ well-being.
Here is an excerpt from the investigation titled “Not Medically Necessary”: Inside the Company Helping America’s Biggest Health Insurers Deny Coverage for Care:
EviCore markets itself to insurance companies by promising a 3-to-1 return on investment — that is, for every $1 spent on EviCore, the insurer would pay out $3 less on medical care and other costs. EviCore salespeople have boasted of a 15% increase in denials, according to the investigation, which is based on internal documents, corporate data and dozens of interviews with former employees, doctors, industry experts, health care regulators and insurance executives. Almost everybody interviewed spoke on condition of anonymity because they continue to work in the industry.
To accomplish this “3-to-1 return”, EviCore increasingly denies prior authorization requests, with its denial rates in states like Arkansas reaching nearly 20%, much higher than even the 7% denial rate in Medicare Advantage. Insurers don’t explicitly ask for more denials, but their focus on “controlling the spend” leads to this outcome. And it’s not just EviCore. The reporters found that other companies, like Carelon Medical Benefits Management, engage in similar practices, with the same financial incentives to deny care to protect their bottom line.
These profit-driven denials often have devastating consequences for patients like John Cupp, a 61-year-old Ohio man whose doctor requested a heart catheterization to assess his worsening heart condition. EviCore denied it, twice, forcing Cupp to settle for a cheaper, less effective test.
Cupp’s case is not an isolated incident. In 2022, HEALTH CARE un-covered published an anonymously-authored piece by a former industry executive who ran a prior authorization shop. The executive wrote:
The other hidden cost of the prior authorization program, one that never seemed to factor into this calculation of return on investment, is patient impact. For every procedure we clinically review and determine to be medically unnecessary, we’ve created an opportunity for confusion and frustration for patients. They likely had no idea that there was an independent arbiter paid by their insurance company to review their doctor’s decisions regarding their health.
These instances of confusion and frustration are what drive the majority of the bad publicity within the industry, and rightfully so. Without an ability to communicate directly with patients, it is very hard to explain why their doctor may have been mistaken or outdated in their referring practices, or even that their doctor just forgot to submit all the paperwork necessary for a review. As a result, patients are left feeling like a faceless corporation is making their medical decisions and undermining their actual doctors.
ProPublica and Capitol Forum’s investigation into EviCore sheds light on a disturbing reality: Health insurance corporations increasingly rely on third-party companies with incentives to deny care.
While prior authorizations were originally intended to prevent unnecessary treatments and overbilling, those third-party companies have twisted the process into a profit-generating machine, one that forces patients and doctors to jump through hoops to secure even the most basic medical services. The result is a system where care all too often is denied to patients who need it most while insurers and their partners reap the financial rewards.
]]>
Last week, the Senate Permanent Subcommittee on Investigations, led by Sen. Richard Blumenthal (D-Connecticut), released a Majority Staff Report on rampant prior authorization (PA) abuses in Medicare Advantage (MA). The report offers unique insight into recent trends in the use of prior authorization by Medicare Advantage plans and the strategy and motives behind insurance corporations’ use of it.
While the findings won’t surprise those who’ve been following health policy trends, it is immensely concerning that between 2019 and 2022, the prior authorization denial rate for post-acute care in UnitedHealth’s Medicare Advantage plans doubled. The denial rate for long-term acute care hospitals in Humana’s Medicare Advantage plans increased by 54% from 2020 to 2022. During this time, UnitedHealth, CVS/Aetna, and Humana increased their use of artificial intelligence (AI) for prior authorization reviews, often resulting in increasing denial numbers and decreasing (or absent) review time by human beings.
The report recommends that the Centers for Medicare and Medicaid Services (CMS) collect additional data, conduct audits of prior authorization processes, and expand regulations on the use of technology in PA reviews. While these recommendations would be positive steps, the report’s findings call into question whether Big Insurance can ever be trusted or regulated enough to prevent abuse of patients through prior authorization and other mechanisms.
This report provides an in-depth look at insurers’ motivations. Sadly, those motivations are not to “make sure a service or prescription is a clinically appropriate option,” as UnitedHealth claims, but to decrease the amount spent on medical care to increase the corporations’ profits. The report noted that CVS, which owns Aetna, saved $660 million in 2018 by denying Medicare Advantage patients’ claims for treatment at inpatient facilities. Around the same time, CVS found in its testing of a model to “maximize approvals,” which would be a good thing for patients, that the model jeopardized profits because it would lead to more care being covered. In 2022, CVS “deprioritized” a plan to increase auto-approvals because of the lost “savings” from denying patient care.
The report found that the motivation to increase profits, without regard for patient care, was not unique to CVS/Aetna. UnitedHealth’s naviHealth subsidiary provided this directive to its employees: “IMPORTANT: Do NOT guide providers or give providers answers to the questions” when speaking to a patient’s doctor about a prior authorization request. Instead of working collaboratively with doctors to get patients the care they need, UnitedHealth told its workers not to bother. In a training session offered to Humana employees involved in prior authorization reviews, the company explained that reviewers should deny a request for post-acute care even if a patient needed more intensive treatment. Humana told reviewers that the lack of an in-network lower-level care facility for patients to go to was not a reason to approve post-acute care and that usually the situations can be “sorted out,” presumably by the patient with no help from the insurer.
All three companies (UnitedHealth, Humana and CVS/Aetna), which dominate the Medicare Advantage program, demonstrated a striking lack of motivation to protect and enhance patient care, instead showing a primary motivation to increase profits and margins.
The subcommittee’s report also noted that UnitedHealth, CVS/Aerna, and Humana are increasingly using AI to make care decisions and cutting humans, especially doctors, out of the process. The researchers found that in 2022, UnitedHealth looked into how using AI and machine learning could aid in predicting which denials of post-acute care requests were most likely to be overturned. One would hope this effort would be to decrease the number of wrongfully denied prior authorization requests and increase patient access to care.
However, the report includes a quote from a recap of a meeting on the project asking “what we could do in the clinical review process to change the outcome of the appeal,” meaning that UnitedHealth was interested in preventing the overturning of denials, not getting the decision right in the first place. The report also found evidence that naviHealth used artificial intelligence to help determine the coverage decisions for a patient’s post-acute care claim before any human post-acute care providers evaluated a case. The report’s authors found that denials for post-acute care facilities rose rapidly once naviHealth began managing these requests for UnitedHealth’s MA plans.
These are just some of the findings in the 54-page report on Big Insurance’s use of prior authorization to deny Medicare Advantage patient requests for post-acute care. The report’s findings demonstrate the abuse of prior authorization by the insurers, the motivation to increase profit and decrease patient care, and the use of AI to increase denials. Further, the findings underscore that prior authorization is a tool used by Big Insurance primarily to maximize profits. The report puts forward recommendations to cut down on abusive denials, which would have some positive impact. More importantly, I believe the report provides more evidence that it is becoming exceedingly less likely that private and for-profit insurance companies can be regulated and act in a way that promotes patient health over profits.
]]>
New polling from Data Progress shows that voters are very concerned about Republicans’ health care policy proposals, as laid out in Project 2025, for a possible second Trump term.
As we have covered previously in HEALTH CARE un-covered, Project 2025 would radically change health care in this country. It would make it less affordable and accessible, roll back benefits that millions of American families rely on every day, and impose dangerous abortion bans.
The plan would also lead to the end of traditional Medicare — handing it over exclusively to Big Insurance to generate profits for Wall Street investors.
Many of these proposals stem from Republican policy priorities that have been around for decades, but the sweeping nature of Project 2025 and the prospect of a president and Congress who support these proposals have put them back into focus.
And that is why new polling from Data Progress is so important and revealing. The polling finds that voters have deep concerns about Project 2025’s health care proposals, including:
77% of voters are concerned about privatizing Medicare
76% of voters are concerned about repealing the policy that capped insulin costs at $35 or less per month
75% of voters are concerned about the plan to cut spending on Medicaid
And this is not a partisan issue. The polling shows deep concern about these proposals from Independents and Republicans, not just Democrats. The poll found:
74% of independents and 63% of Republicans are concerned about privatizing Medicare
76% of independents and 62% of Republicans are concerned about repealing the cap on insulin in Medicare
77% of independents and 61% of Republicans are concerned about cutting spending on Medicaid
In today’s polarized political environment, these are staggering numbers and show how deeply unpopular these proposals are.
Ultimately, voters will render their verdict on Project 2025 at the ballot box in less than two weeks. But as we inch closer to Election Day, this polling shows that voters have deep concerns about how Republicans would likely handle health care, one of the top concerns of voters, in a second Trump term.
Danielle Deiseroth is the Executive Director of Data for Progress. Since joining the team in 2020, Danielle has led dozens of public opinion research projects at the national, state, and congressional district levels.
Dental insurance is a corner of our costly, inefficient health care system that does not get enough spotlight. And before you tell me that you have great dental insurance through your employer or your spouse, hear me out.
First, some basics about dental insurance:
Most states do not regulate medical loss ratios when it comes to dental plans. What is a medical loss ratio, or ‘MLR’ if you’re into health care insider speak? It’s the percentage of insurance premiums (the money we pay for our insurance) that must be spent on patient care and not on company overhead – including the salaries, bonuses, and other compensation paid to executives and employees of an insurance company. This means that in your state, chances are good that dental insurance companies do not have to spend much of the money they rake in from your payments on your dental costs and can pocket an exorbitant amount for themselves.
For an example, I invite you to research California Delta Dental and their executives’ salaries. The company’s 25 executives are paid more than $500,000 per year with the CEO pulling in $9.5 million annually – and they are all smiles!
Second, if you’ve ever had a dental procedure beyond a cleaning or basic cavity filling, you know that dental events can often cost $1,000 or more. Well, most dental insurance companies cap your annual benefit at between $1,000-$2,000, so your insurance doesn’t go a very long way for you if you need a crown, a root canal, or God forbid, a dental implant. Even with that great dental insurance you think you have, you’ll be paying out of pocket for any non-minor treatment. I know, because even with the Cadillac dental plan, I spent over $15,000 on these services last year. And the benefit maximums have barely budged in over a decade. Seems a bit unfair, given the salaries your premiums are likely paying according to the link above, right?
And third, people don’t always realize that high-quality dental care is critical to overall health. Many chronic diseases can be traced to poor dental health, but not enough regulatory attention is given to dental insurers.
I recently went for a preventive dental visit here in California, the land of millionaire dental insurance executives. The cost, including cleaning, was $250. My dental plan states that my premiums cover two cleanings per year, yet when I filed my claim, it was initially rejected.
No clerical error or reason was provided. It took me multiple phone calls and re-sending receipts just to finally gain reimbursement from my dental insurer. Something tells me that is a feature and not a bug in that particular insurance company’s process. (It’s not Delta Dental). I did the math and they could cover 156,567 cleanings with what they pay their executives each year, but I’m only asking for one (maybe two if I can squeeze it in later this year).
Gotta make sure their Vice President of Profit “Extraction” can afford to dock his boat in San Francisco Bay, I guess.
]]>